The Study in Brief
-
The lack of access to family physicians is a critical issue in Canada, with millions of Canadians lacking access to a primary care provider. Shortages have been exacerbated by the pandemic, which led to notable levels of physician burnout and an increase in retirements.
-
This Commentary estimates the shortages of family physicians in provinces and territories, and analyzes the contributing factors, from stress and paperwork to an ageing doctor demographic, outdated payment models and restrictive quotas on internationally trained talent.
-
While necessary, simply increasing the number of family physicians will not suffice to meet the demands of a growing and ageing population. Optimizing the utilization and efficiency of existing physicians is critical. In addition, significant changes to the organization and funding of care delivery – as well as expanding the scope of other primary care providers – will be necessary to meet current and future care demands.
-
Addressing the primary care access gap involves five strategies, all of which the provinces are pursuing to varying degrees. They are: 1) expanding the number of training positions and filling the unfilled residency spots with international medical graduates; 2) reducing the administrative burden for family physicians; 3) providing alternate payment models; 4) expanding the scope of practice of other primary care providers; and 5) expanding team-based models of care. Sharing best practices across the country and adapting successful strategies from other provinces can inform policies aimed at enhancing primary care coverage and access.
The author thanks Rosalie Wyonch, Parisa Mahboubi, Mawakina Bafale, John Richards, Ake Blomqvist, Trisha Hutzul and anonymous reviewers for helpful comments on an earlier draft. The author retains responsibility for any errors and the views expressed.
Introduction
Primary care is the foundation of the Canadian health system.1 Primary care providers are often the first contact for patients accessing the medical system; they diagnose and treat illness, manage chronic diseases, promote health, and provide comprehensive care to individuals. They are also responsible for coordinating care between patients and different specialists. Health systems with strong primary care provision have better health outcomes (Macinko et al. 2003, Starfield et al. 2005), lower emergency use (Niti and Ng 2003), lower hospitalizations (van Loenen et al. 2014, Wolters et al. 2017), lower mortality (Macinko et al. 2003), lower costs (Starfield and Shi 2002), better chronic disease management (Starfield et al. 2005), and exhibit greater equity (Berchet and Guanais 2019).
However, many Canadians struggle with access to care: about 4.6 million (14 percent) Canadians aged 12 and older did not have a regular healthcare provider in 2022 (Statistics Canada 2023a). Compared to the national average, Prince Edward Island (24.1 percent), Quebec (21.3 percent) and Newfoundland and Labrador (18.1 percent) had a higher proportion of residents who claimed to have no regular healthcare provider. Additionally, about 6.6 million Canadians had a family doctor aged 65 and over (Glazier 2023), meaning that even more people could be without primary care access due to retirements. In 2022, a national survey by OurCare showed that one in five people reported not having a family doctor or nurse practitioner (approximately 6.5 million Canadians2). Traditionally underserved populations – those with low income (Mangin et al. 2022), new immigrants (Turin et al. 2020), and Indigenous people (Statistics Canada 2023b) – were among the least likely to report having a regular primary care provider.
For those without a family physician,3 walk-in clinics (in-person and virtual) and emergency departments become a default option – or they go without any care at all. In 2023, 38 percent of Canadians reported that they went to the emergency department for a condition that could be treated at a regular place of care (CIHI 2024).4 The use of emergency departments to treat minor health problems leads to inefficient use of hospital resources and higher healthcare costs. For example, in 2022/23 in Ontario, lower-acuity patients accounted for 23 percent (or 1.29 million) of all emergency department visits (OAGO 2023). Some of these patients sought emergency care unnecessarily due to the absence of a primary care provider or immediate alternatives. Notably, the direct cost of an emergency department visit in Ontario was approximately $165 per visit, nearly three times greater than the cost of primary care, which was about $56 per visit. Furthermore, Canadians grappling with chronic conditions such as diabetes, hypertension, depression, or psychosis may end up in emergency departments for care management in the absence of a primary care provider.
More than one in five people without a regular primary care provider (21 percent) reported paying a fee for the care they received the last time.5 This out-of-pocket pay was most common in Quebec, where 37 percent reported paying such fees.6 Among Canadians who had a regular healthcare provider in 2023, only 23 percent said they could get an appointment on the same, or the next, day when they were sick or needed medical attention – the lowest reported percentage among the 10 developed countries included in a Commonwealth Fund study (CIHI 2024). This represents a significant drop from the 2020 survey result wherein 41 percent of survey respondents in Canada indicated they could get a same or next day appointment. As a result, we can conclude both access to care and timeliness are deteriorating in Canada.
Timely access to care is essential to Canadians. All Canadians should have access to primary care, especially those who live in rural and remote areas and underserved communities. Improving family health services is the first of four shared health priorities for the new $25 billion in funding (over 10 years) for provincial/territorial governments (Health Canada 2024).7
Each province is at varying stages of implementation across five policy strategies that could improve primary care access:
• expanding the number of training positions for prospective family doctors and accelerating pathways for international medical graduates to enter family medicine, whether direct-to-practice or through access to residency positions;
• reducing the administrative burden for family physicians;
• providing alternate payment models;
• expanding the scope of practice of other primary care providers; and
• expanding team-based models of care.
Sharing best practices and adapting successful strategies across provinces will be essential to improving primary care coverage and access across Canada.
Supply of Family Physicians
Family physician supply in Canada has fluctuated over time. In the 1980s, the average annual growth rate in the number of family physicians was 3.94 percent, contributing to a perceived surplus of physicians (Figure 1). In the 1990s, a number of policies significantly limited the growth of physician supply. For example, the provincial and territorial ministers of health implemented significant reductions to medical school enrollments, postgraduate medical training, and recruitment of international medical graduates; all to control rising healthcare expenditures (Barer et al. 1991, Marchildon and Di Matteo 2023). Other policies that had an impact on the supply of family physicians included: elimination of the one-year rotating internship and implementation of a two-year family medicine residency as a minimum requirement for practice; an increase in the ratio of specialist to family medicine residency positions; and social and economic policies that resulted in an exodus of physicians to the US (Chan 2002, Malko and Huckfeldt 2017). As a result of these policies, the net inflow of physicians into the physician practice pool dropped from 1,040 physicians per year in the period of 1990-1993, to 313 physicians per year in the period 1994-2000 (Chan 2002). This resulted in 5,093 fewer physicians entering the practice pool, compared to what would have been expected if this inflow rate had not dropped. The average annual growth rate of family physicians in the 1990s was 0.61 percent (Figure 1).
In the early 2000s, provincial and territorial decision-makers reversed the restrictive policies and expanded entry to medical schools as shortages of physicians in rural and remote areas became apparent. However, due to the time delay – from medical school admission to becoming a practicing physician – it took several years to see an increase in the number of practicing physicians as a result of these changes. In the 2000s, the average annual growth rate of family physicians increased to 1.92 percent (Figure 1).
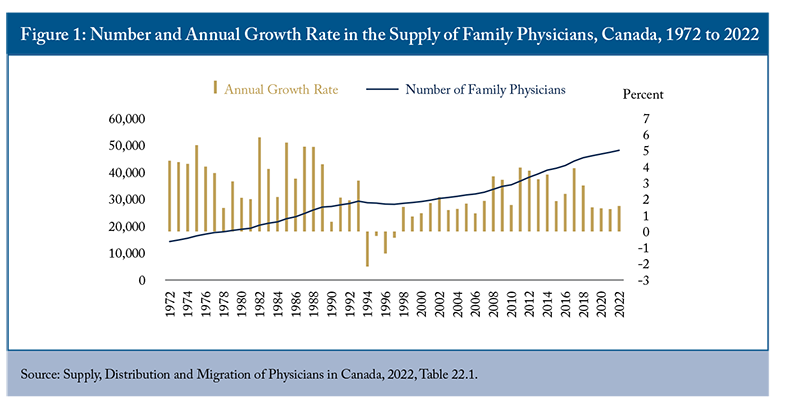
Historically, the annual growth rate in the number of family physicians consistently exceeded that of the population, except during the 1990s (see online Appendix A1). However, since 2018, the growth rate of family physicians has slowed, averaging around 1.75 percent (see Figure 1) and in 2022 the growth rate of the population surpassed that of family physicians. While the population grew by 1.84 percent, the number of family physicians only increased by 1.58 percent, thus compounding the issue of access to primary care.
Meanwhile, the pandemic exacerbated the shortage of family physicians. Younger family physicians under age 55 were more likely to experience stress, emotional distress, and burnout (Gunja et al. 2022). Half or more of older family physicians reported they would stop seeing patients within the next three years. The National Physician Health Survey found that 57 percent of general practitioners surveyed experienced burnout in 2021, marking a 24-percentage point increase from 2017, and rates of dissatisfaction were higher for general practitioners than for specialists (CMA 2021). More than half of general practitioners were likely or very likely to reduce or modify their clinical hours in the next two years. This reduction in working hours leaves the remaining family physicians with higher caseloads, more stress, and less time to care for increasingly complex patient needs. Many family physicians want to retire, reduce workloads, or leave the profession. In the first six months of COVID-19, twice as many family physicians stopped practicing in Ontario compared to previous years (Kiran et al. 2022a).
Family Physician Shortages in Canada
As discussed, shortages of family physicians are prevalent in Canada. This being the case, how many family physicians do we need for today, and for the years to come?
Based on the number of family physicians available in 2022 and the number of Canadians with access to care, each active family physician provided care to an estimated average of 695 patients.8
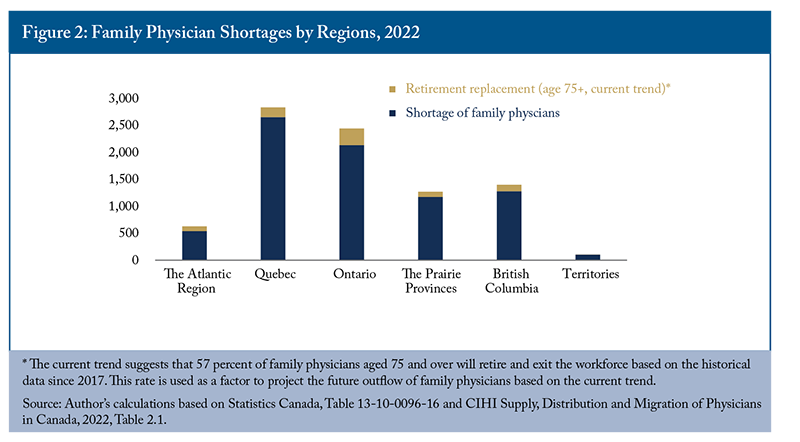
Given the current population without access to primary care, an additional 7,844 family physicians would be required to address the current access gap.9 If we suppose the annual growth rate of family physicians remains at the current 1.6 percent, filling the gap would take about 10 years – an unattainable prospect especially considering increasing demand due to population growth and ageing.
Figure 2 shows the shortage of family physicians in each region in 2022. Among all provinces, Quebec needs the most family physicians to fill their care gap, at 2,658. Ontario also has a shortage of 2,136 family physicians, but it also needs to hire at least an additional 526 family physicians to replace its retiring physicians (see online Appendix B for methodology).10 Otherwise, more Ontarians will be left without a primary care provider once their existing physicians choose to retire. According to the Ontario College of Family Physicians (2023), by 2026 one in four Ontarians (or 4.4 million) are expected to be without a family doctor.
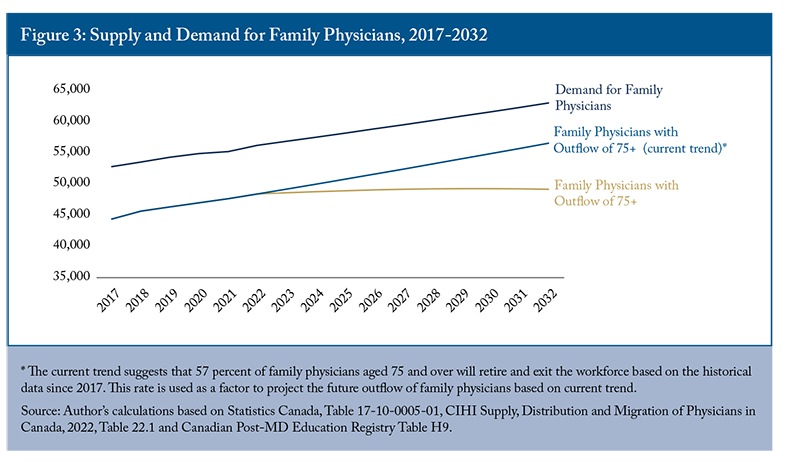
The future demand for family physicians will only increase. The federal government’s ambitious immigration target, set out in 2022, called for 1.5 million more immigrants to Canada over the next three years, contributing to population growth. Canada’s population is predicted to increase by 12 percent (38.9 million to 43.6 million) from 2022 to 2032.11 Over that same period, the number of existing trainees is expected to increase by approximately 37 percent, but the number of retiring family physicians aged 75 and over rises by 66 percent. Under the normal retirement scenario – where 57 percent of family physicians aged 75 and over retire – the projected supply of family physicians in 2032 will be sufficient to meet 90 percent of the demand for that year (Figure 3). However, if all family physicians aged 75 and over were to retire, only 78 percent of the projected demand would be met and the shortage of family physicians in 2032 would increase to 13,845 (online Appendix B). With only about 1,550 family physicians exiting residency in 2022, Canada’s current pipeline of family medicine graduates will not be sufficient to meet this future demand.12
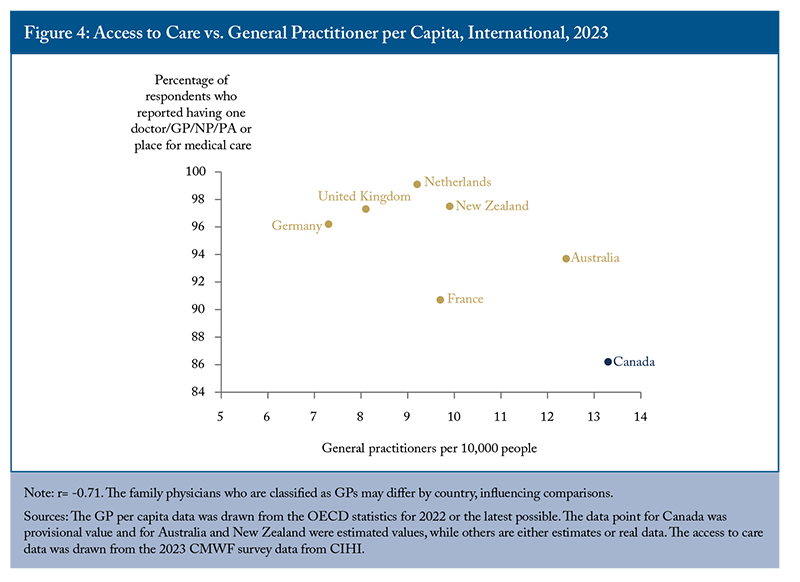
How Canada Compares: Lessons from Abroad
Compared to other Commonwealth Fund countries,13Canada’s performance in primary care has been consistently weak, particularly in access to care. Of 10 countries, Canada ranked the worst in having a doctor or a regular place for medical care: 86.2 percent of surveyed Canadians reported having a regular doctor/GP/NP/PA or place for medical care in 2023 (CIHI 2024).14 However, Canada had the highest number of general practitioners (GPs) per 10,000 population in 2022, at 13.3 (Figure 4).15 In contrast, the Netherlands only had 9.2 GPs per 10,000 population, but 99 percent of its survey respondents reported having a doctor or place for medical care. Indeed, Figure 4 suggests that a higher density of family physicians per capita may not be associated with better primary care access.16 Shehaed et al. (2023) find that countries “with high rates of primary care attachment have stronger contractual agreements and accountability for family physicians, including where they practise, their scope of practice, and who they accept as patients.” In comparison, most family physicians in Canada operate as independent contractors, with no inherent obligation or accountability for the services they provide to the health insurer, namely, the provincial/ territorial governments. Countries such as the Netherlands either mandate registration for patients with a general practitioner, or strongly support it. Their primary care systems offer valuable lessons for Canada (e.g., online Appendix C, and Tan et al. 2023). The federal and provincial governments should refine primary care policies by learning from international best practices to enhance primary care and elevate Canada’s ranking among high-performing countries.
Contributing Factors to Family Physician Shortages
Many factors contribute to family physician shortages in Canada, including an ageing physician workforce, reduced interest in family medicine among new medical students, administrative burdens, and changes in physician practices that have resulted in decreased efficiency.
The workforce of family physicians is older than other occupations, indicating that higher rates of retirement can be expected in the coming decades. As older doctors retire, many cannot find younger colleagues to take over their practices.
The proportion of family physicians aged 60 and over rose from 11.85 percent in 2001 to 26.06 percent in 2017 (online Appendix A2). Meanwhile, the proportion of those under 39 has declined since the 1990s. Between 1992 and 2002, this proportion decreased from 45 to 28.6 percent and continued in this manner until 2008, although it began to increase slowly thereafter. In 2011, the proportion of family physicians aged 60 and over surpassed those under 39 for the first time, and did so for the three subsequent years. Although this trend has reversed since 2014, the gap has been very small. This suggests that the influx of new family physicians may not be able to keep pace with the outflow of older physicians, potentially impacting access to primary care services.
More broadly speaking, in 2022, there were 48,199 family physicians in Canada (CIHI 2023a). The average age of family physicians in Canada was 49.3 in 2022, ranging from 48 in Saskatchewan to 51.1 in Quebec (CIHI 2023a). Close to a quarter of family physicians (11,871) were aged 60 and over.
There were 13,369 young family physicians under 39, accounting for 27.74 percent of the workforce, slightly higher than the proportion of senior family physicians (Figure 5).
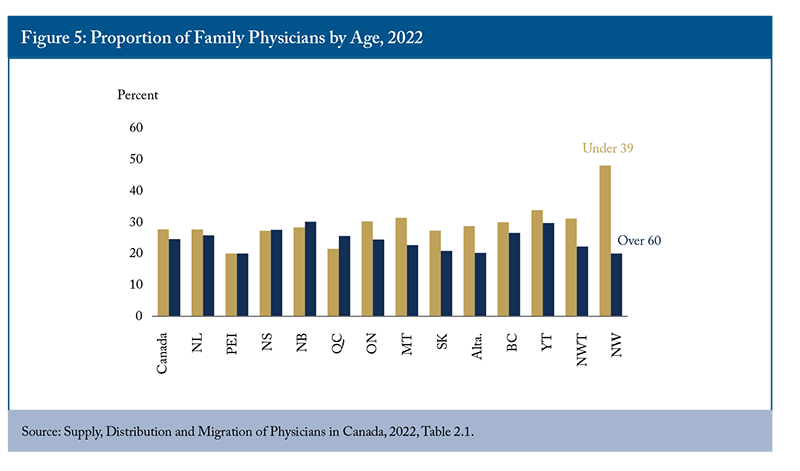
Among provinces, New Brunswick and Yukon had the highest share of family physicians aged 60 and over, at around 30 percent, followed by Nova Scotia and British Columbia. In Nova Scotia, New Brunswick, and Quebec there were more senior family physicians than young physicians, highlighting the significant issue of an ageing physician population in these provinces.
Reduced Interest in Family Medicine
Fewer and fewer medical students are interested in family medicine. The significant gap in compensation between family physicians and specialists could be one of the contributing factors influencing medical students to pursue residencies in specialties other than primary care. On average, family physicians made about $83,000 less than medical specialists and $208,000 less than surgical specialists in 2021-22 (CIHI 2023c). In 2023, 30.3 percent of Canadian medical graduates ranked family medicine as their first-choice discipline in the first iteration, down from 38 percent in 2015. This reflects a growing uncertainty among medical trainees about whether family medicine is a viable career choice. Even after graduating in family medicine, some individuals may choose not to practice comprehensive family medicine. A recent survey from the University of Alberta found that only 38.8 percent of surveyed residents were willing to take on a patient panel (roster) in the next five years, compared to 72.6 percent prior to entering residency, indicating a change in resident practice intentions (Horvey et al. 2023). Kabir et al. (2021) found that residents and early-career family physicians opt for specialized practices (e.g., emergency department, hospitalist, palliative care or sports medicine) instead of comprehensive practices due to “self-preservation within the current structure of the healthcare system, support from colleagues, training experiences in medical school and/or residency.” Therefore, increasing the number of young family physicians and encouraging them to take more patients, through various supports such as team-based care, are critical.
In addition, unfilled family residency spots have been increasing. The 2023 Canadian Resident Matching Service (CaRMS 2023) showed that 6 percent of family medicine residency spots in Canada were unfilled (100 positions, mainly in Quebec). Other medical disciplines had only one unfilled residency position in 2023. The number of unfilled family residency spots in Quebec has increased over time (Wittevrongel and Shaw 2022), likely due to its French language requirements and restrictions in practice. According to Wittevrongel and Shaw (2022), Quebec’s bureaucratic licensing and accreditation process also prevents the mobility of physicians from other provinces and abroad.
Meanwhile, hundreds of international medical graduates are interested in family medicine but lack residency spots. According to CaRMS (2023), 1,060 international medical graduates applied for residency positions in family medicine in 2023. Just 364 were matched with the necessary post-graduate training, a match rate of 34.3 percent compared to 97.8 percent for Canadian medical graduates. Barriers that prevent IMGs from filling vacant residency positions and complicate the matching process include a restrictive quota for IMGs during the initial matching process and varying regulatory and language prerequisites across provinces. With a few residency positions available to IMGs, Canada is limiting its supply of family physicians and underutilizing its medical talent.
In Canada, most family physicians are independent small business owners fully responsible for all the staffing and infrastructure costs needed for their practices (Glazier 2023). In addition to looking after their patients, family physicians also need to manage payroll, equipment, supplies, and other administrative tasks. According to the Canadian Medical Association (2021), nearly half of family physicians surveyed spent 10 to 19 hours per week on administrative tasks. A recent survey from the Ontario College of Family Physicians (2023) also indicated that, on average, Ontario family physicians work an average of 47.7 hours per week, with 40 percent of that spent on administrative tasks. Some administrative tasks include sending duplicate forms requested from different organizations, writing unnecessary sick notes, and filling out lengthy insurance forms that are different for each company. Enhancing data linkages and utilizing administrative data instead of duplicating efforts offers a pathway to reducing administrative workload.
These administrative tasks can result in time and productivity losses. For instance, physicians across Canada are spending 18.5 million hours every year on unnecessary administrative work, equivalent to 55.6 million patient visits (Alegbeh and Jones 2023). About two-thirds of this work could be completed by another health professional, and a third could likely be eliminated. The administrative burden also affects physicians’ job satisfaction (Gajjar et al. 2022), increases their burnout, and worsens their mental health. More than half of primary care physicians in Canada were not satisfied at all with the amount of time they spent on administrative work in 2022 (CIHI 2023b). Close to one-third (28.8 percent) plan to stop seeing patients regularly in the next one to three years. About two-thirds of family physicians in Ontario are also planning to make a change or leave the profession in the next five years (OCFP 2023).
Instead of the traditional small-business model of family medicine, younger medical graduates prefer to be employees with benefits such as paid vacation and parental leave (Hedden et al. 2021). They do not want to run their own clinics, hire staff, and have the administrative burden of being a business owner and providing indirect patient care. More and more young family physicians want a higher quality of work-life balance. They also prefer to work in inter-professional group practices where they can get support from teammates.
Although family physician supply in Canada has been increasing in recent years, physician productivity has decreased and average hours worked per week have declined, resulting in a net reduction of physician services per capita (Lee, Mahl, and Rowe 2021). Crossley, Hurley and Jeon (2009) observed a decline in patient care hours across all age cohorts of physicians. They found that the changing behaviour of male physicians contributed more significantly to the overall decrease in direct patient care hours compared to the growing proportion of female family physicians in the physician workforce. They argue that increasing direct patient care hours by 5 percent among current practicing physicians would have a greater impact on effective physician supply than substantial increases in medical school enrollments. Similarly, Kralj, Islam and Sweetman (2024) found that although average physician payments have risen over the past three decades, the average weekly hours worked by physicians have consistently decreased. Since 1997, male physicians’ work hours have notably declined, while their female counterparts’ hours have remained relatively stable at around 45 hours per week. In particular, male physicians accounted for 5.7 of the overall 6.9-hour decrease in work hours. According to Kralj, Islam and Sweetman (2024), male physicians’ preferences to a better work-life balance are a main contributing factor.
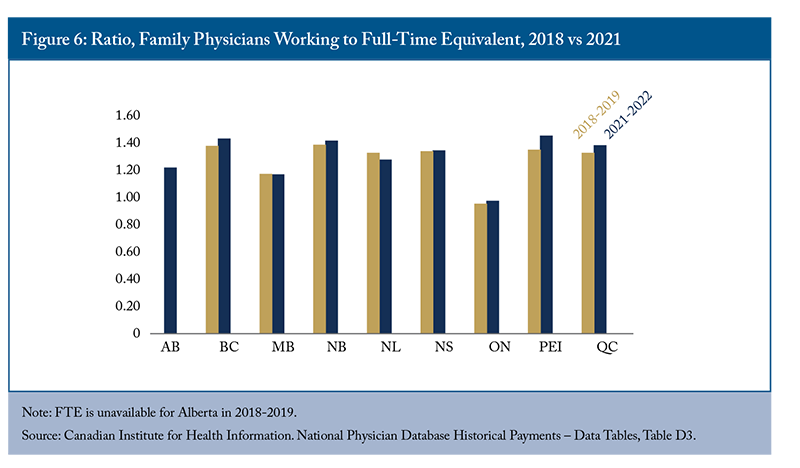
Although Canada has 48,199 family physicians, many work part-time and some who are licensed may perform little to no clinical work, focusing on research or holding administrative positions. To produce a more meaningful measurement of physician supply, the concept of counting Full-Time Equivalent (FTE) physicians was adopted.17Comparing the headcount of physicians to the estimated number of FTE physicians provides insights into provincial variations in physician practices (Wyonch 2021). Compared to three years ago, the ratio of family physicians working to the FTE standard has increased in all provinces in 2021-2022, except Manitoba and Newfoundland and Labrador (Figure 6). Prince Edward Island, British Columbia, and Quebec experienced the greatest increases in this ratio. These provinces have 1.4 times as many family physicians as estimated full-time equivalents.
As noted in Wyonch (2021), family physicians in Ontario generally work the equivalent of full-time clinical hours, making it the only province where this is the case. Despite the fact that British Columbia and Quebec saw increases of 624 and 580 family physicians, respectively, their FTE numbers only increased by 254 and 122. This discrepancy suggests that, on average, fewer clinical services were provided, despite having more family physicians eligible to practice in these provinces. This implies that there is potential to improve patient access to primary care by increasing the hours worked by existing family physicians and decreasing the amount of time they spend on non-patient care. Increasing the use of both team-based models of care and other primary care providers would also help with primary care access, something that will be discussed in the following sections.
Policy Strategies to Improve Primary Care
Addressing primary care access gaps requires a multifaceted approach. Simply increasing the number of family physicians will not suffice to meet the demands of a growing and ageing population. Canada already has a higher density of family physicians than comparator countries that achieve better outcomes in terms of population access. Similarly, the density of family physicians in Canada has grown over time, but access to primary care remains a challenge for a significant portion of the population. Provinces need to focus on improving the efficiency of primary care to enhance patient access. This involves reducing administrative burdens, implementing alternate payment models, expanding the scope of practice of other primary care providers, and promoting team-based models of care.
Increasing Training Positions for Prospective Family Doctors and Accelerating Pathways for IMGs
The number of residency spots needs to be expanded and pathways for international medical graduates (IMGs) to enter family medicine need to be accelerated, whether through access to residency positions or direct-to-practice. In 2023, universities and family medicine residency programs increased the number of available positions by 60 (CaRMS 2023). The total number of students matching to family medicine increased by 59. Two-thirds of this increase came from IMGs. IMGs matching to family medicine increased from 439 in 2022 to 555 in 2023. This increase in IMG matching implies that most regions (except Quebec) have the potential to match more IMGs if they increase the residency spots for IMGs. Correspondingly, the number of practicing physicians who can mentor graduates needs to increase to provide residency training.
The United Kingdom has relied on IMGs for years, with 50 percent of its doctors being international graduates in 2021 (General Medical Council 2022). Since government initiatives opened more training spots, the UK witnessed its general practice trainees grow by 34 percent, with IMGs filling most of these additional places. On average, about a third of Canada’s family physicians are foreign-trained (31.1 percent), with Quebec having the lowest proportion of foreign doctors at just 7.8 percent. Seventy-three out of 100 unfilled residency spots in 2023 were in Quebec.18 Quebec needs to better use its agreement with France and streamline applications of French doctors to increase the inflow of family physicians (Wittevrongel and Shaw 2022). Allowing more IMGs to practice in Canada could also help alleviate the significant physician shortage in underserviced areas, since most IMGs entering postgraduate training in Canada sign a “return of service” commitment, obliging them to practice in an underserviced community for a number of years after completion of residency, depending on the province (Malko and Huckfeldt 2017).
Streamlining credential recognition for internationally trained physicians (ITPs) is also important to boost the supply of family physicians. ITPs need to go through a lengthy credential recognition process, assessment exams, and residency training.19 With limited residency spots available for IMGs, it will likely take a few years for ITPs to utilize their medical training and skills.
Some provinces are already moving in the right direction to streamline recognition of foreign credentials and work experience. For example, nine provinces offer practice-ready assessments (PRAs), a path for internationally trained family physicians who have already completed their residency.20Ontario renewed its funding for the PRA program in June, and New Brunswick launched the program in October last year. Still, the number of assessments seems low: only 50 applicants in Ontario and 10 applicants in New Brunswick will be accepted.21 Research has shown that investments in skills assessment (such as PRAs) and residency training opportunities for IMGs can generate real annual rates of return between 9 and 13 percent by streamlining professional recognition (Emery et al. 2007).
Eliminating Unnecessary Administrative Burdens
Reducing the administrative burden for family physicians can improve care, reduce burnout, and free up time better spent on direct patient care. Alegbeh and Jones (2023) find that 38 percent of administrative work for physicians is unnecessary and could be eliminated or streamlined. It includes sick notes, insurance forms, excessive hospital documentation, etc. Nova Scotia is the only government that has committed to reducing physician red tape by 10 percent, roughly 50,000 hours, by 2024 (Alegbeh and Jones 2023). If jurisdictions across Canada committed to reducing physician administrative burden by 10 percent, as Nova Scotia has done, they could free up approximately 1.9 million hours of physician time – equivalent to more than 5.5 million patient visits (Alegbeh and Jones 2023).
Learning from Nova Scotia, other jurisdictions should measure the total administrative burden of their family physicians and identify the portion of administrative work that can be done by others or eliminated. Two measures from Nova Scotia’s Patient Access to Care Act are worth mentioning: limiting sick notes to long-absent employees, and allowing the government to prescribe Workers Compensation Board forms and documents.22Other jurisdictions should also eliminate employer requirements for sick notes for short-term illness. In addition, they need to standardize insurance forms across public and private insurers and simplify social program and benefit forms. It is necessary to conduct an internal analysis of the requirements for provincial social programs and evaluate areas where duplication of information can be eliminated and forms can be streamlined. For example, they can further utilize digital tools to facilitate autofill and the sharing of forms among family physicians and social services.
Jurisdictions should also mandate standardized referral forms within a specialty across provinces. There are many forms across different specialty areas, each using different formats and requesting similar information in varying ways. The use of e-referral with central intake, and a single common queue for specialty care and advanced imaging, could reduce administrative burden for family physicians.
Moreover, the use of AI can have a positive impact on primary care, such as supporting routine task completion and enhancing clinical decision support. Ontario recently announced a pilot project aimed at the safe use of AI, allowing for the automatic summarization or transcription of patient conversations into electronic medical notes with their consent.23However, the implementation of AI in primary care must carefully address several considerations. These include: ensuring alignment with the needs of primary care providers; mitigating potential threats to clinical skills and capacity; addressing broader concerns surrounding ethical, legal, and social implications of AI utilization; ensuring transparency and control over data; and establishing mechanisms for co-creation, leveraging high-quality data, and evaluating the efficacy of AI tools (Terry et al. 2022).
Implementing Alternate Payment Models
Implementing physician payment reform may facilitate change in organization and delivery of care. However, it is important to develop mechanisms for accountability when introducing such reforms.
Traditionally, primary care services are paid on a fee-for-service (FFS) basis; each family physician is paid at a specified rate for each service provided. Such a payment model incentivizes physicians to increase the volume of services they provide, thus potentially over-treating patients and reducing the time and quality of patient interactions (Blomqvist and Busby 2012, Blomqvist and Wyonch 2019).
An alternative is the capitation model, where physicians are paid per patient based on patients’ socioeconomic characteristics.
Research finds that the capitation model is effective at “containing rising costs, increasing the quality of care, enabling higher patient satisfaction and better adherence to medication and treatment protocols” (Berchet and Guanais 2020). Compared to pure FFS, either capitation or a blended model better uses total health system resources (Blomqvist and Busby 2012). Physicians in the capitation model tend to enroll more patients (Glazier et al. 2009). However, capitation models in Ontario unintentionally incentivize family physicians to select less costly and less sick patients (Rudoler et al. 2015). As highlighted by Martin et al. (2021), compensation models need to reflect the complexity of work and diversity of population served by family physicians.
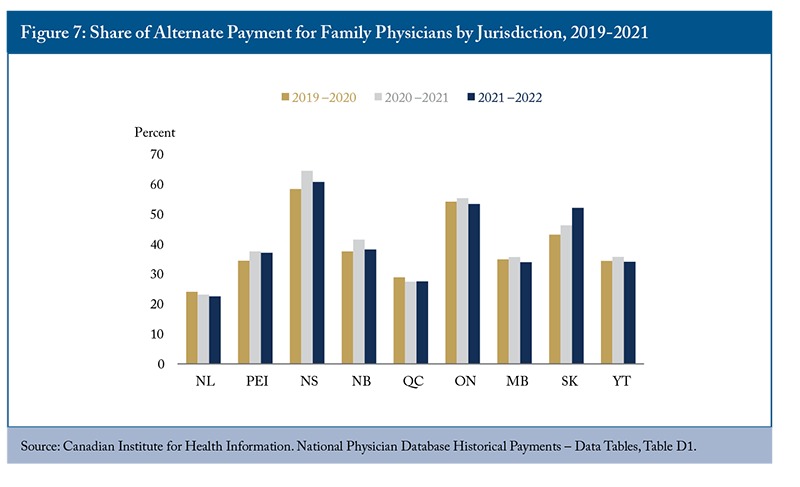
In the past two decades, the implementation of alternate payment models (APPs) has been prevalent in several provinces.24 There is a shift from FFS to APPs in areas such as salary, blended payments, capitation and other contracts. These models have different strengths and weaknesses and may exhibit varying performance levels depending on the context and target population (Tan et al. 2023).
In 2021-2022, FFS accounted for 64 percent of total clinical payments, and alternate payments represented 36 percent. The split has been stable at the pan-Canadian level in the last decade, with some jurisdictional variations. Among nine jurisdictions where data are available, Nova Scotia is leading in paying their family physicians with alternate payment, at 61 percent (Figure 7), followed by Ontario (53 percent) and Saskatchewan (52 percent). However, FFS remains the dominant payment model for family physicians in British Columbia (81 percent, CIHI 2023d). 25
APPs need to be further developed and applied, and Canada can draw valuable lessons in this from countries like Norway and the Netherlands (online Appendix C). They include bundled payments for chronic disease management, or performance-based incentives to improve access and hold their physicians accountable. Shahaed et al. (2023) found that general practitioners in countries with high rates of primary care attachment “have contractual arrangements and accountability to government, insurers or both.” Standards of accountability for timely access include public reporting of patient experience measures. Tan et al. (2023) reviewed 11 jurisdictions (i.e., six international countries and five Canadian provinces) and found that only England, Scotland and US-Kaiser Permanente have regularly used patient surveys as accountability measures. In contrast, there is a notable lack of accountability measures for quality improvement in Canada. When introducing primary care payment reforms, governments need to carefully design the incentive mechanism, hold family physicians accountable for the services delivered, monitor performance, and support quality improvement (Tan et al. 2023). For example, requirements for shadow billing2626 help facilitate routine monitoring and evaluation, and strengthening enforcement of contractual obligations such as after-hours care could be beneficial (Tan et al. 2023).2727 Currently, GPs paid through APPs in Nova Scotia adhere to an accountability framework that includes measures such as conducting shadow billing (subject to audit) and submitting an annual activity report detailing their activities beyond shadow billing.
Expanding the Scope of Practice of Other Primary Care Providers
Making the best use of existing health professionals, such as nurse practitioners (NPs) and pharmacists, can improve primary care access and free up family physicians’ time to treat more patients. Having interprofessional clinicians work in team-based care with family physicians ensures comprehensive care with increased continuity and coordination of care.
NPs can provide primary care services such as diagnosing and treating illnesses, ordering and interpreting diagnostic tests, prescribing medication, and making referrals to specialists. However, their scope of practice varies across Canada (CIHI 2020b). Since 2021, several provinces have lifted the restrictions for NPs to utilize a fuller range of their skills. As NPs can roster and manage patients, increasing the number of NPs can reduce the pressure on the supply of family physicians. There were 8,206 NPs in Canada in 2022, with a growth rate of 10.9 percent.28 To increase the number of NPs, Canada needs to increase its nursing base and improve the growth rate of RNs (1.1 percent in 2022). Otherwise, the nursing shortage will become worse as more registered nurses become NPs.
Provincial governments need to make better use of NPs. In Ontario, over 25 NP-led clinics provide primary care to nearly 80,000 people in rural areas and Northern Ontario, where the shortage of family physicians is more acute (Ontario Health 2023). British Columbia and New Brunswick have also started to utilize NP-led clinics to address the gap in primary care. Rickards and Hamilton (2020) found that people who see an NP rather than a physician in New Brunswick expressed high levels of satisfaction with both the care they received and the improved accessibility to healthcare providers. However, only 5 percent of people in Canada reported having an NP as their primary care clinician, and 31 percent indicated that their primary care practice included an NP. Some NPs are underemployed in rural and remote communities or underutilized in urban hospitals.292The remaining regulatory and remuneration obstacles that hinder NPs’ ability to practice need to be addressed. For example, Alberta’s government is creating a new compensation model for NPs to encourage them to operate independently and increase comprehensive primary care services in the community.30
Over the past few years, pharmacists have been able to do more for their patients, such as assessing common aliment symptoms and prescribing medications for minor ailments (Canadian Pharmacists Association 2023a). However, pharmacists in many provinces are still underutilized. Alberta is the only province allowing pharmacists to practice to their fullest scope (Canadian Pharmacists Association 2023b). Other provinces are making some progress. For example, Nova Scotia has introduced pharmacist-delivered primary care (i.e., Community Pharmacy Primary Care Clinics) for 31 minor ailments, and allows pharmacists to provide treatment for people with common chronic conditions like diabetes and asthma.31 Ontario and British Columbia have also enabled pharmacists to prescribe some medications.32
Allowing pharmacists to prescribe drugs and make certain treatment decisions can alleviate restrictions on access to treatment. Expanding their scope of practice helps them build relationships with their patients, know their medication history, and provide better care for their patients. Governments need to continue expanding pharmacists’ scope of practice in consultation with healthcare professionals.
Expanding Team-based Models of Primary Care
In team-based models of primary care, family physicians work with nurses, nurse practitioners, pharmacists, social workers, dietitians, and other allied healthcare professionals to achieve high-quality, coordinated care.
Recent literature has shown that team-based care improves healthcare quality, use, costs, and the health outcomes of chronically ill patients (Reiss-Brennan et al. 2016, Blomqvist and Wyonch 2019, Pany et al. 2021, Mangin et al. 2022). Patients enrolled in team-based care models were more likely to receive recommended diabetes care and experience more improvements in care over time (Kiran et al. 2015). Team-based practices also reduce physician exhaustion and improve satisfaction with the work (Willard-Grace et al. 2014). During the pandemic, Ontario’s Family Health Teams could continue in-person and virtual care (Ashcroft et al. 2021) while many solo practices stalled. Wait times to access team members have also reduced due to virtual care adoption (Donnelly et al. 2021). Team-based primary care, coupled with payment reform, can also improve patient outcomes and reduce emergency department use (Kiran et al. 2022b). For example, under the capitation-based alternate funding model, two clinics in Alberta that used team-based care have saved the health system $120 million over the past 10 years, mainly from reduced emergency department visits and inpatient visits (Health Quality Council of Alberta 2019). The finding shows that the capitation-based funding model plays a key factor in enabling the structure and organization of team-based care.
In the last two decades, each province has adopted different team-based practices. However, the expansion of team-based primary care has been heterogeneous and slow. According to Aggarwal et al. (2023), team-based practices “varied in physician payment, the types of providers, group size, governance models, requirements for patient enrollment, the scope of services providers, and the nature of the population served.” Online Appendix D provides a summary of the prevalence of team-based care models in each province and their respective coverage. Alberta has the highest proportion of residents enrolled in team-based care, at 85 percent. Many provinces have just started team-based care where data are not available. Ontario was an early adopter of team-based care, with 187 Family Health Teams (FHTs) along with other forms of inter-professional team-based care currently running. However, despite the potential benefits, less than 25 percent of Ontarians receive team-based primary care.33The full population potential of team-based care remains untapped in Ontario. Research suggests that team-based practices have a lower average number of patients per physician compared to non-team practices, indicating the capacity for increased patient enrollment in existing team-based models (Kiran 2015). A successful FHT should be able to accommodate more patients than an individual family physician. For example, Windsor FHT has 100-125 solo primary care practitioners but serves approximately 200,000 people (Ontario Ministry of Health 2019), with each primary care practitioner caring for an average of about 2,000 people.
Canada needs to improve and scale up team-based care (Bell et al. 2023). It is favoured by both family physicians and patients; nearly 70 percent of surveyed physicians supported team-based care (Hedden et al. 2021), while the majority of surveyed Canadians (90 percent) also felt very comfortable or comfortable getting care from another primary care provider on the team if their family doctor or nurse practitioner recommends it.34
To further the transition to team-based care, provinces need to address financial, structural, governance, and accountability barriers (Farmer et al. 2022). While expansion is essential, increasing physician capacity, monitoring and measuring results, and continuous quality improvement are also critical (Lukey et al. 2022).35 The evaluation of team-based care needs to focus on patient-reported outcomes such as access, care coordination, prevention and health promotion, and support for managing chronic conditions. Continuous evaluation of each practice can also help improve and refine the model. Governments need to dedicate funding to team-based care and ensure teams add patient capacity and reduce burnout (Bodenheimer 2022). They also need to minimize duplication of skills, optimize productivity, and foster teamwork among primary care providers so each can work to their potential (Drummond et al. 2022). The decision-makers and providers of team-based care would also benefit from appropriate leadership providing clarity of purpose, goals, roles, scopes of practice, and procedures throughout the health system (Suter et al. 2017, Wranika et al. 2019, Farmer et al. 2022).
The Current Picture
Closing the primary care access gap is a priority across provinces, with each province at varying stages of implementing the aforementioned five strategies. The following table illustrates the progress of 10 provinces in enhancing primary care since 2022 (see online Appendix E for more information). In general, primary care is moving in a positive direction in Canada, with British Columbia, Nova Scotia, and Ontario having made the most significant progress. Nova Scotia stands out as the sole province that has made advancements on all fronts. Conversely, Quebec lags behind, having implemented the fewest initiatives to enhance primary care access. This highlights the urgent need for significant action in Quebec to address its primary care access challenges.
Green highlights indicate that the provincial government took actions directly on the strategy, for example by increasing the number of family physicians or setting a goal to reduce administrative burden. Yellow indicates provinces taking initiatives relevant to the strategy, for example establishing a working group or expanding financial incentives. Red shows no actions taken since 2022.
Many provinces, with the exception of Alberta and Quebec, are increasing residency spots to increase the supply of family physicians. Many provinces are also expanding the scope of practice of other primary care providers, which is a good step forward. However, provinces such as Manitoba and Newfoundland and Labrador need to consider adopting their own context-based strategy.
Only four provinces have created or expanded alternate payment models since 2022: Alberta, British Columbia, Nova Scotia, and Saskatchewan. Several provinces have introduced incentives to attract and retain family physicians. While commendable, holding family physicians accountable for the services they provide is crucial to seeing improvement in patient access.
Among all areas for improvement, reducing the administrative burden does not appear to be a priority for many provinces. While Nova Scotia introduced the Patient Access to Care Act to reduce physician paperwork, only British Columbia and Manitoba are establishing working groups to tackle the same issue.
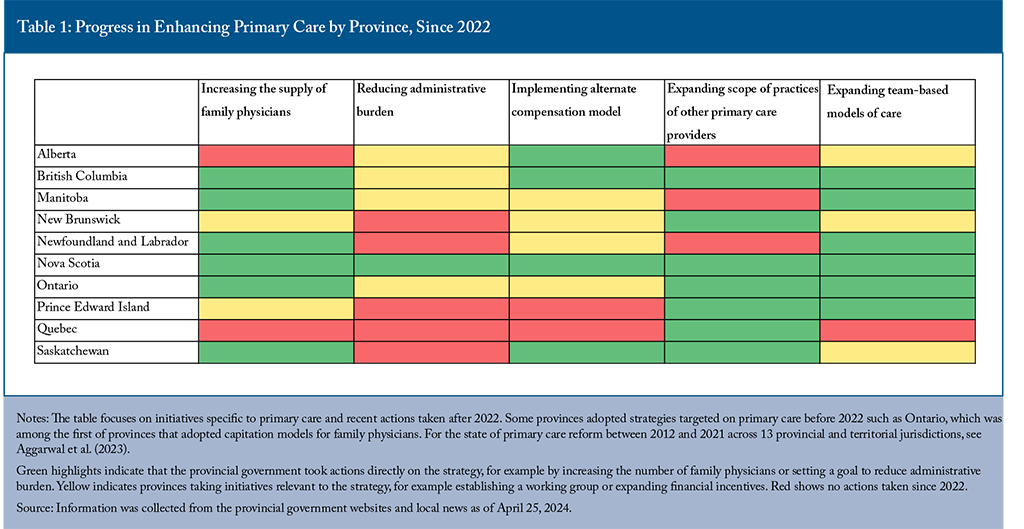
Ontario, Quebec, and Newfoundland and Labrador have also taken positive steps to reduce red tape in healthcare; however, effective measurement and the establishment of reduction targets are necessary to enact tangible improvements for physicians and healthcare overall (Loeppky, Yoo, and Alegbeh 2024).
Ongoing measurement and evaluation of these initiatives is important, especially with clearly defined outcome indicators such as the percentage of people attached to primary care. Evaluation requires regular and reliable information about care access, emphasizing the importance of health data and transparency within and across provinces. While most provinces are expanding team-based care, its productivity and administrative efficiency need to be evaluated (Drummond et al. 2022). Governments need to support family physicians while holding them accountable for system-wide goals, such as access and patient outcomes, to facilitate improvement over time.
In the Northern territories where family physicians are few, and the turnover rates are high, making the best use of nurses by expanding nurse-led community health centers or clinics could help alleviate the shortage of physicians. Increasing the adoption of virtual care shows promise in enhancing primary care access and fostering team collaboration across geography (Bhatia and Falk 2018, Flood, Thomas and McGibbon 2023). Peixoto et al. (2024) found that integrated virtual care can connect previously unattached patients in rural and underserved Ontario communities to a family physician, delivering comprehensive team-based primary care. The pandemic has led to a significant surge in virtual care adoption, with two-thirds of health systems transitioning to virtual platforms. In 2023, 32.3 percent of Canadians received healthcare from a primary care provider through telehealth, surpassing the Commonwealth Fund country average of 23 percent (CIHI 2024). Among those who used virtual care with their primary care provider, the majority of them (80 percent) reported satisfaction with their experience. To fully leverage virtual care’s potential, especially in rural and remote areas, significant investments in broadband infrastructure are essential. Ensuring accessibility of virtual tools for older adults, visible minorities, and Indigenous communities also requires thoughtful design to enhance user experience.
Some provinces and territories, including Newfoundland and Labrador,36Prince Edward Island,37 Nova Scotia,38and Quebec, have made significant investments in increasing care access through virtual care. Many primary care physicians now provide a range of online services, such as email consultation, appointment scheduling, and prescription renewals. By utilizing virtual care effectively, governments can leverage its potential to reduce healthcare costs, increase patient convenience and create health system capacity (Bhatia et al. 2020). Other jurisdictions should consider expanding these pilot initiatives to modernize our health system.
Conclusion
Since the pandemic, provinces and territories have been actively working to improve primary care access. While increasing the supply of family physicians remains a priority, optimizing the utilization and efficiency of existing physicians is also critical. A comprehensive approach that combines strategies such as increasing the inflows of family physicians, streamlining administrative processes, implementing alternate payment models, expanding the scope of practice of other primary care providers, and expanding team-based models of care is essential for significant progress.
As the federal government engages in bilateral agreements with provincial governments, there is sufficient funding available for primary care innovations. However, it is imperative to implement ongoing performance measurement, quality improvement, and accountability mechanisms for policy innovations, all with transparent public reporting. The federal government needs to collect comprehensive data to track the provincial initiatives after implementation, especially in Ontario, British Columbia, and Nova Scotia. Incorporating patient-reported measures can further enhance health service delivery and effectiveness. Moreover, the federal government needs to facilitate the improvement and coordination of primary care initiatives between provinces. This involves identifying and disseminating best practices related to regulation, compensation, governance, and other pertinent factors. Continuous cross-provincial comparisons are necessary to ensure ongoing learning and improvement in primary care access across Canada.
References
Aggarwal, Monica, Brian Hutchison, Reham Abdelhalim, and G. Ross Baker. 2023. “Building High-Performing Primary Care Systems: After a Decade of Policy Change, Is Canada ‘Walking the Talk?’” The Milbank Quarterly 101(4): 1-52.
Alegbeh, Alchad, and Laura Jones. 2023. “Patients Before Paperwork: Nova Scotia’s Approach to Improving Patient Care by Reducing Physician Red Tape.” Canadian Federation of Independent Business. Available at https://www.cfib-fcei.ca/en/research-economic-analysis/patients-before-paperwork-nova-scotias-approach-to-improving-patient-care-by-reducing-physician-red-tape
Ashcroft, Rachelle, Catherine Donnelly, Sandeep Gill, Maya Dancey, Simon Lam, Allan K. Grill, and Kavita Mehta. 2021. “The Delivery of Patient Care in Ontario’s Family Health Teams during the First Wave of the COVID-19 Pandemic.” Health Policy 17(2): 72–89.
Barer, M. L., and Gregory Lloyd Stoddart. 1992. “Toward Integrated Medical Resource Policies for Canada: background document.” Canadian Medical Association Journal 146(3): 347-351.
Bell, Bob, Georgina Black, Jodi Butts, Vivek Goel, Alika Lafontaine, Victoria Lee, David MacNaughton, Danielle Martin, and Jane Philpott. 2023. “Taking Back Health Care.” Public Policy Forum. Available at https://ppforum.ca/wp-content/uploads/2023/01/TakingBackHealthcare-Jan2023-PPF-EN-1.pdf
Berchet, Caroline, and Frederico Guanais. 2020. “Realising the Potential of Primary Health Care.” OECD. Available at https://www.oecd-ilibrary.org/sites/a92adee4-en/index.html?itemId=/content/publication/a92adee4-en
Bhatia, R. Sacha, Trevor Jamieson, James Shaw, Carole Piovesan, Leah T. Kelley, and William Falk. 2020. Canada’s Virtual Care Revolution: A Framework for Success. Commentary 586. Toronto: C.D. Howe Institute. Available at https://www.cdhowe.org/sites/default/files/2021-12/Commentary_586.pdf
Blomqvist, Åke, and Colin Busby. 2012. How to Pay Family Doctors: Why “Pay per Patient” is Better than Fee for Service. Commentary 365. Toronto: C.D. Howe Institute. Available at https://www.cdhowe.org/sites/default/files/attachments/research_papers/mixed/Commentary_365.pdf
Blomqvist, Åke, and Rosalie Wyonch. 2019. Health Teams and Primary Care Reform in Ontario: Staying the Course. Commentary 551. Toronto: C.D. Howe Institute. Available at https://www.cdhowe.org/sites/default/files/2021-12/Commentary percent20551.pdf
Bodenheimer, Thomas. 2022. “Revitalizing Primary Care, Part 2: Hopes for the Future.” Annals of Family Medicine 20(5): 469–478.
Canadian Pharmacists Association. 2023a. “Common Ailment Prescribing in Canada.” Available at https://www.pharmacists.ca/advocacy/practice-development-resources/common-ailments/
________________. 2023b. “Pharmacists’ Scope of Practice in Canada.” Available at https://www.pharmacists.ca/advocacy/scope-of-practice/
Canadian Institute for Health Information. 2020. “Nurse Practitioner Scopes of Practice Vary across Canada’s Provinces and Territories” [infographic].
________________. 2023a. “Supply, Distribution and Migration of Physicians in Canada, 2022 – Historical Data.”
________________. 2023b. “Survey Results Reveal the Challenges Experienced by Family Doctors.” Available at https://www.cihi.ca/en/survey-results-reveal-the-challenges-experienced-by-family-doctors
________________. 2023c. “A Profile of Physicians in Canada.” Available at https://www.cihi.ca/en/a-profile-of-physicians-in-canada
________________. 2023d. National Physician Database – Payments Data, 2021–2022.
________________. 2024. “How Canada Compares: Results From the Commonwealth Fund’s 2023 International Health Policy Survey of the General Population Age 18+ in 10 Countries – Data Tables.” Available at https://www.cihi.ca/en/commonwealth-fund-survey-2023
Canadian Medical Association. 2021. “National Physician Health Survey.” August. Available at https://www.cma.ca/sites/default/files/2022-08/NPHS_final_report_EN.pdf
Canadian Resident Matching Service (CaRMS). 2023. “2023 CaRMS Forum.” Available at https://www.carms.ca/pdfs/carms-forum-2023.pdf
Crossley, Thomas F., Jeremiah Hurley, and Sung-Hee Jeon. 2009. “Physician Labour Supply in Canada: A Cohort Analysis.” Health Economics 18(4):437-56.
Donnelly, Catherine, Rachelle Ashcroft, Nicole Bobbette, Christine Mills, Amanda Mofina, Todd Tran, Kyle Vader, Ashley Williams, Sandeep Gill, and Jordan Miller. 2021. “Interprofessional Primary Care during COVID-19: a Survey of the Provider Perspective.” BMC Family Practice 22(1): 31.
Duong, Diana, and Lauren Vogel. 2023. “Ontario, Quebec and Alberta lead record family medicine residency vacancies.” Canadian Medical Association Journal 195(15): E557-E558. Available at https://doi.org/10.1503/cmaj.1096047
Drummond, Don, Duncan Sinclair, and Jillian Gratton. 2022. Troubles in Canada’s Health Workforce: The Why, the Where, and the Way Out of Shortages. Commentary 630. Toronto: C.D. Howe Institute. Available at https://www.cdhowe.org/sites/default/files/2022-11/Commentary percent20630.pdf
Emery, John C Herbert, Rodney A. Crutcher, and Alexandra Harrison. 2007. “Social Rates of Return to Investment in Skills Assessment and Residency Training of International Medical Graduates in Alberta.” Health Policy 79(2-3):165-74.
Farmer, Julie, Albert, M., Sarah Carbone, Monika Roerig, and Sara Allin. 2022. “Improving Access to High Quality Team Based Primary Care in Rural/Remote/Northern Canada.” North American Observatory on Health Systems and Policies. Rapid Review #35.
Flood, Colleen M., Bryan Thomas, and Ella McGibbon. 2023. “Canada’s Primary Care Crisis: Federal Government Response.” Healthcare Management Forum 36(5):327-332.
Gajjar, Jainita, Naomi Pullen, Yin Li, Sharada Weir, and James G Wright. 2022. “Impact of the COVID-19 Pandemic upon Self-reported Physician Burnout in Ontario, Canada: Evidence from a Repeated Cross-sectional Survey.” BMJ Open 12(9).
General Medical Council. 2022. “The Workforce Report 2022: The State of Medical Education and Practice in the UK.” Available at https://www.gmc-uk.org/-/media/documents/workforce-report-2022---full-report_pdf-94540077.pdf
Glazier, Richard H. 2023. “Our Role in Making the Canadian Health Care System One of the World’s Best.” Canadian Family Physician 69(1):11-16. Available at https://doi.org/10.46747/cfp.690111
Glazier, Richard H., Julie Klein-Geltink, Alexander Kopp, and Lyn M. Sibley. 2009. “Capitation and Enhanced Fee-for-service Models for Primary Care Reform: A Population-based Evaluation.” Canadian Medical Association Journal 180(11): E72-E81. Available at https://doi.org/10.1503/cmaj.081316
Gunja, Munira Z., Evan D. Gumas, Reginald D. Williams II, Michelle M. Doty, Arnav Shah, and Katharine Fields. 2022. “Stressed Out and Burned Out: The Global Primary Care Crisis.” The Commonwealth Fund. Available at https://www.commonwealthfund.org/publications/issue-briefs/2022/nov/stressed-out-burned-out-2022-international-survey-primary-care-physicians
Health Canada. 2024. “Working together to improve health care in Canada: Overview.” Available at https://www.canada.ca/en/health-canada/corporate/transparency/health-agreements/shared-health-priorities.html
Health Quality Council of Alberta. 2019. “Crowfoot and Taber Clinics – Case Study Evaluation.” Available at https://hqca.ca/reports/crowfoot-and-taber-clinics-case-study-evaluation/
Hedden, Lindsay, Setareh Banihosseini, Nardia Strydom, and Rita McCracken. 2021. “Family Physician Perspectives on Primary Care Reform Priorities: a Cross-Sectional Survey.” Canadian Medical Association Journal 9(2):E466-E473. Available at https://doi.org/10.9778/cmajo.20200102
Horvey, Samantha, Lauren J Eastman, and Tina Korownyk. 2023. “RE: Changes Over Time in Patient Visits and Continuity of Care Among Graduating Cohorts of Family Physicians in 4 Canadian Provinces.” Canadian Medical Association Journal. Available at https://www.cmaj.ca/content/re-changes-over-time-patient-visits-and-continuity-care-among-graduating-cohorts-family
Islam, Rabiul, Boris Kralj, and Arthur Sweetman. 2023. “Physician Workforce Planning in Canada: The Importance of Accounting for Population Aging and Changing Physician Hours of Work.” Canadian Medical Association Journal 195(9) E335-E340. Available at https://doi.org/10.1503/cmaj.221239
Kabir, Monisha, Ellen Randall, Goldis Mitra, M Ruth Lavergne, Ian Scott, David Snadden, Lori Jones, Laurie J Goldsmith, Emily G Marshall, and Agnes Grudniewicz. 2021. “Resident and Early-career Family Physicians’ Focused Practice Choices in Canada: a Qualitative Study.” Healthcare Management Forum 36(5):327-332.
Kiran, Tara, Alexander Kopp, Rahim Moineddin, and Richard H. Glazier. 2015. “Longitudinal Evaluation of Physician Payment Reform and Team-based Care for Chronic Disease Management and Prevention.” Canadian Medical Association Journal 187(17) E494-E502. Available at https://doi.org/10.1503/cmaj.150579
Kiran, Tara, Michael E. Green, Fangyun Wu, Alexander Kopp, Lidija Latifovic, Eliot Frymire, Rahim Moineddin, and Richard H. Glazier. 2022a. “Family Physicians Stopping Practice During the COVID-19 Pandemic in Ontario, Canada.” The Annals of Family Medicine 20(5):460-463.
Kiran, Tara, Rahim Moineddin, Alexander Kopp, and Richard H. Glazier. 2022b. “Impact of Team-Based Care on Emergency Department Use.” The Annals of Family Medicine 20(1):24-31. Available at https://doi.org/10.1370/afm.2728
Kralj, Boris, Rabiul Islam, and Arthur Sweetman. 2024. “Long-term Trends in the Work Hours of Physicians in Canada.” Canadian Medical Association Journal 196(11): E369-E376. Available at https://doi.org/10.1503/cmaj.231166
Lee, Shoo K., Sukhy K. Mahl, and Brian H. Rowe. 2021. “The Induced Productivity Decline Hypothesis: More Physicians, Higher Compensation and Fewer Services.” Healthcare Policy 17(2):90-104.
Loenen, Tessa van, Michael J van den Berg, Gert P Westert, and Marjan J Faber. 2014. “Organizational Aspects of Primary Care Related to Avoidable Hospitalization: a Systematic Review.” Family Practice 31(5): 502-516. Available at https://doi.org/10.1093/fampra/cmu053
Loeppky, Keyli, SeoRhin Yoo, and Alchad Alegbeh. 2024. “Patients before Paperwork Jurisdictional Update: Canadian Progress on Reducing the Physician Administrative Burden.” Canadian Federation of Independent Businesses. Available at https://www.cfib-fcei.ca/hubfs/research/reports/2024/2024-02-Patients-before-paperwork-Update.pdf
Macinko, James, Barbara Starfield, and Leiyu Shi. 2003. “The Contribution of Primary Care Systems to Health Outcomes within Organization for Economic Cooperation and Development (OECD) Countries, 1970-1998.” Health Service Research 38(3):831-65.
Malko, Andrei, and Vaughn Huckfeldt. 2017. “Physician Shortage in Canada: A Review of Contributing Factors.” Global Journal of Health Science 9.
Mangin, Dee, Kamila Premji, Imaan Bayoumi, Noah Ivers, Azza Eissa, Sarah Newbery, Liisa Jaakkimainen, Dominik A. Nowak, Michael Green, Susan Beazley, Andrew Pinto, Victoria Haldane, Elizabeth Muggah, Jennifer Rayner, David M. Kaplan, Onil Bhattacharyya, Allan K. Grill, Nicolas S. Bodmer, Anna Perkhun, Beth Cowper-Fung, Riva E. Levitan, Cathy Mastrogiacomo, Steve Nastos, Prabhjot Sangha, Matthew J. Schurter, James Wright, Jose M. Valderas, Karen B. Born, Fahad A. Razak, Richard H. Glazier, Tara Kiran, and Danielle Martin. 2022. “Brief on Primary Care Part 2: Factors Affecting Primary Care Capacity in Ontario for Pandemic Response and Recovery.” Ontario COVID-19 Science Advisory Table. Available at https://doi.org/10.47326/ocsat.2022.03.68.1.0
Marchildon, Gregory, and Livio Di Matteo. 2023. “Physician workforce planning and boom–bust economic cycles: a retrospective on the Barer–Stoddart report.” Canadian Medical Association Journal 195(4): E162-E165. Available at https://doi.org/10.1503/cmaj.221611
Martin, Danielle, Bob Bell, Georgina Black, Jodi Butts, Beth Cowper-Fung, Vivek Goel, Alika Lafontaine, David MacNaughton, Kwame McKenzie, Jane Philpott, Jake Starratt-Farr, and Verna Yiu. 2023. “Primary Care for Everyone.” Public Policy Forum. Available at https://ppforum.ca/wp-content/uploads/2023/04/PrimaryCareForEveryone-PPF-April2023-EN.pdf
McLeod, Logan, Gioia Buckley, and Arthur Sweetman. 2016. “Ontario Primary Care Models: a Descriptive Study.” Canadian Medical Association Journal 4(4): E679-E688. Available at https://doi.org/10.9778/cmajo.20160069
Ministry of Health. 2019. “A Healthy Ontario: Building a Sustainable Health Care System.” Available at https://www.ontario.ca/document/healthy-ontario-building-sustainable-health-care-system/chapter-3-ten-recommendations-improve-health-care
Mitra, Goldis, Agenes Grudniewicz , M. Ruth Lavergne, Renee Fernandez, and Ian Scott. 2021. “Alternative Payment Models: A Path Forward.” Can Fam Physician 67(11):805-807.
Niti, M., and T P Ng. 2003. “Avoidable Hospitalisation Rates in Singapore, 1991-1998: Assessing Trends and Inequities of Quality in Primary Care.” Journal of Epidemiology Community Health 57(1):17-22.
Newfoundland and Labrador College of Family Physicians. 2018. “Family Medicine in Newfoundland & Labrador: A Ten Year Vision.” Available at https://nl.cfpc.ca/ten-year-vision/
Office of the Auditor General of Ontario. 2016. “Value-for-Money Audit: Physician Billing.” Available at https://www.auditor.on.ca/en/content/news/16_summaries/2016AR percent20summary percent203.11.pdf
________________. 2023. “Value-for-Money Audit: Emergency Departments.”Available at https://www.auditor.on.ca/en/content/annualreports/arreports/en23/AR_emergencydepts_en23.pdf
Ontario College of Family Physicians. 2023. “More Than Four Million Ontarians Will Be Without a Family Doctor by 2026.” November. Available at https://ontariofamilyphysicians.ca/news/more-than-four-million-ontarians-will-be-without-a-family-doctor-by-2026/
Ontario Health. 2023. “Your Health: A Plan for Connected and Convenient Care.” Available at https://www.ontario.ca/page/your-health-plan-connected-and-convenient-care#section-4
Pany, Maximilian J., Lucy Chen, Bethany Sheridan, and Robert S. Huckman. 2021. “Provider Teams Outperform Solo Providers in Managing Chronic Diseases and Could Improve the Value of Care.” Health Affairs 40(3):435–444.
Peixoto, Cayden, Jonathan Fitzsimon, Lisa Hawkins, and Judy Hill. 2024. “Assessing New Patient Attachment to An Integrated, Virtual Care Programme in Rural Primary Care.” Canadian Journal of Rural Medicine 29(1): 7-12.
Reiss-Brennan, Brenda, Kimberly D. Brunisholz, Carter Dredge, Pascal Briot, Kyle Grazier, Adam Wilcox, Lucy Savitz, and Brent James. 2016. “Association of Integrated Team-based Care with Health Care Quality, Utilization, and Cost.” Journal of the American Medical Association 316(8):826–834.
Rickards, Tracey, and Sharon Hamilton. 2020. “Patient Experiences of Primary Care Provided by Nurse Practitioners in New Brunswick, Canada.” The Journal for Nurse Practitioners 16(4): 299-304. Available at https://doi.org/10.1016/j.nurpra.2019.12.027
Richardson, Ben, and Yadullah Hussain. 2022. “Canada Needs More Doctors—and Fast.” RBC Thought Leadership. November. Available at https://thoughtleadership.rbc.com/proof-point-canada-needs-more-doctors-and-fast/
Rudoler, David, Audrey Laporte, Janet Barnsley, Richard H. Glazier, and Raisa B. Deber. 2015. “Paying for Primary Care: A Cross-sectional Analysis of Cost and Morbidity Distributions across Primary Care Payment Models in Ontario Canada.” Social Science & Medicine 124: 18-28.
Rudoler, David, Sandra Peterson, David Stock, Carole Taylor, Drew Wilton, Doug Blackie, Fred Burge, Richard H. Glazier, Laurie Goldsmith, Agnes Grudniewicz, Lindsay Hedden, Margaret Jamieson, Alan Katz, Adrian MacKenzie, Emily Marshall, Rita McCracken, Kim McGrail, Ian Scott, Sabrina T. Wong, and M. Ruth Lavergne. 2022. “Changes over Time in Patient Visits and Continuity of Care among Graduating Cohorts of Family Physicians in 4 Canadian Provinces.” Canadian Medical Association Journal 194:1639-1646.
Schultz, Susan E. and Richard H. Glazier. 2017. “Identification of physicians providing comprehensive primary care in Ontario: a retrospective analysis using linked administrative data.” Canadian Medical Association Journal 5(4): E856-E863.
Shahaed, Heba, Richard H. Glazier, Michael Anderson, Erica Barbazza, Véronique L.L.C. Bos, Ingrid S. Saunes, Juha Auvinen, Maryam Daneshvarfard, and Tara Kiran. 2023. “Primary care for all: lessons for Canada from peer countries with high primary care attachment.” Canadian Medical Association Journal 195(47): E1628-E1636. Available at https://doi.org/10.1503/cmaj.221824
Starfield, Barbara, and Leiyu Shi. 2002. “Policy Relevant Determinants of Health: an International Perspective.” Health Policy 60(3):201-18.
Starfield, Barbara, Leiyu Shi, and James Macinko. 2005. “Contribution of Primary Care to Health Systems and Health.” Milbank Quarterly 83(3):457–502.
Statistics Canada. 2023a. Has a Regular Healthcare Provider, by Age Group. Available at https://www150.statcan.gc.ca/t1/tbl1/en/tv.action?pid=1310009616
______________. 2023b. Study: Access to primary health care among First Nations people living off reserve, Métis and Inuit, 2017 to 2020. Available at https://www150.statcan.gc.ca/n1/daily-quotidien/231006/dq231006b-eng.htm
Simkin, Sarah, Simone Dahrouge, and Ivy Lynn Bourgeault. 2019. “End-of-career Practice Patterns of Primary Care Physicians in Ontario.” Canadian Family Physician 65(5):e221-e230. Available at https://www.cfp.ca/content/65/5/e221.long
Suter, Esther, Sara Mallinson, Renee Misfeldt, Omenaa Boakye, Louise Nasmith, and Sabrina T. Wong. 2017. “Advancing team-based primary health care: a comparative analysis of policies in western Canada.” BMC Health Services Research 17(1):493.
Tan, Stefanie, Julie Farmer, Monika Roerig, and Sara Allin, 2023. “Primary Care Governance and Financing: Models and Approaches.” North American Observatory on Health Systems and Policies. Rapid Review #37. Available at https://www.ihe.ca/advanced-search/primary-care-governance-and-financing-models-and-approaches
Turin, Tanvir C., Ruksana Rashid, and Mohammad Lasker. 2020. “Perceived Challenges and Unmet Primary Care Access Needs among Bangladeshi Immigrant Women in Canada.” Journal of Primary Care & Community Health 11. Available at https://doi.org/10.1177/21501327209526
Willard-Grace, Rachel, Danielle Hessler, Elizabeth Rogers, Kate Dubé, Thomas Bodenheimer, and Kevin Grumbach. 2014. “Team Structure and Culture are Associated with Lower Burnout in Primary Care.” Journal of the American Board of Family Medicine, 27(2):229–238.
Wittevrongel, Krystle, and Maria Lily Shaw. 2022. “A Prescription for Quebec’s Doctor Shortage.” Montreal Economic Institute.
Wolters, R., J. Braspenning, and M. Wensing. 2017. “Impact of Primary Care on Hospital Admission Rates for Diabetes Patients: A Systematic Review.” Elsevier Ireland Ltd 129: 182-196. Available at http://dx.doi.org/10.1016/j.diabres.2017.05.001
Wranik, Wiesława Dominika, Sheri Pricec, Susan M. Haydt, Jeanette Edwards, Krista Hatfield, Julie Weir, and Nicole Doria. 2019. “Implications of Interprofessional Primary Care Team Characteristics for Health Services and Patient Health Outcomes: A Systematic Review with Narrative Synthesis.” Health Policy 123(6):550-563.
Wyonch, Rosalie. 2021. Help Wanted: How to Address Labour Shortages in Healthcare and Improve Patient Access. Commentary 590. Toronto: C.D. Howe Institute. Available at https://www.cdhowe.org/sites/default/files/attachments/research_papers/mixed/Commentary_590_0.pdf
- 1 According to Canada Institute for Health Information, primary care involves routine care, care for urgent but minor or common health problems, mental health care, maternity and child care, psychosocial services, liaison with home care, health promotion and disease prevention, nutrition counselling, and end-of-life care.
- 2 OurCare surveyed 9,000 people aged 18 and over and did not include the 12-18 age group that Statistics Canada covered. I expect the reported shortages to be worse if this age group were included. For more information, see https://data.ourcare.ca/all-questions.
- 3 Family physicians refers to both family physicians and general practitioners.
- 4 The trend over time is relatively stable for Canada. In 2016, 41 percent of Canadians reported that they went to the emergency department for a condition that could have been treated at their regular place of care.
- 5 For more details, see Question 17 on https://data.ourcare.ca/all-questions
- 6 Quebec differs from other provinces as it has growing private clinics operating outside the province’s health insurance plan. For further details, see https://www.theglobeandmail.com/canada/article-quebec-family-doctors-pu…
- 7 As of March 2024, all provinces and territories had signed one-on-one deals with the federal government.
- 8 In 2022, the number of family physicians per 100,000 population in Canada was 123.8, which means each family physician would have cared for 808 patients on average, if the whole population had access to primary care. However, that patient volume is overestimated since 14 percent of Canadians indicated having no access to a regular healthcare provider that year.
- 9 Given 14 percent of Canadians having no access to a regular healthcare provider, approximately 5.5 million Canadians did not have a family physician in 2022. Using the average patient volume of 695, an additional 7,844 family physicians would be required to accommodate the existing population and address the access gap.
- 10 As one reviewer noted, the hours of work among family physicians have shifted over time and the complexity of patients served has increased, making it difficult for family physicians to serve rosters of the size of their predecessors. It is true that we cannot plan for one-on-one replacement of the previous and current generation. However, the patient volume of 695 is reasonably low, compared to other international countries such as the Netherlands.
- 11 See online Appendix B for projection methodology.
- 12 he projections did not include nurse practitioners and physician assistants who are salaried and provide primary care as well. To some extent, they may alleviate the shortage of family physicians. There were approximately 8,206 NPs and 1,000 PAs practicing in Canada. The use of NPs will be discussed in a later section.
- 13 The Commonwealth Fund (CMWF) International Health Policy Surveys conduct rolling surveys of seniors, primary care physicians, and the general public in 11 advanced economies: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom and the United States. The 2023 survey did not include Norway.
- 14 GP: General practitioner; NP: Nurse practitioner; PA: Physician assistant. This is the first time the CMWF survey includes all the primary care workforce in access to care.
- 15 By OECD’s definition, general practitioners (or “family doctors”) assume responsibility for the provision of continuing and comprehensive medical care to individuals, families and communities. Besides general practitioners, they also include district medical doctors – therapists, family medical practitioners (“family doctors”), and medical interns or residents specializing in general practice. Therefore, the number of general practitioners per capita will be slightly higher than the family physicians per capita compiled by CIHI that only include active family physicians. Discrepancies exist due to differences in definition.
- 16 One reviewer notes that some family physicians work in the emergency departments, or practice obstetrics and palliative care, so they do not work in longitudinal care and roster patients.
- 17 Gross income per physician is used as a measure of output to model the “full-time equivalent” number of physicians. For further information about methodology of these estimates, see https://www.cihi.ca/sites/default/files/document/national-physician-dat….
- 18 Quebec has been implementing unpopular healthcare reforms in recent years. It forces general practitioners to work more nights and weekends and do on-call shifts in the ER, making the already difficult recruitment of family doctors even more so (Duong and Vogel 2023).
- 19 Nova Scotia was the first province in Canada to allow physicians who received training in the United States to skip certification exams and begin to practice immediately. Ontario has recently made it easier for internationally trained family doctors in the United States, Ireland, Australia, and Britain to practice medicine in the province by removing supervision and assessment requirements.
- 20 PRA assesses internationally trained physicians in a clinical environment over several months by evaluating candidates more practically and thoroughly while expediting their workforce integration. Supervising physicians will assess internationally-trained physicians to gauge their “practice readiness”; successful PRA candidates are granted an independent licence and must practice in an underserved community for two to three years in a “return of service.” At this time, Prince Edward Island, Yukon, Nunavut and the Northwest Territories do not offer practice assessments within the National Assessment Collaboration’s pan-Canadian framework.
- 21 For further details, see https://touchstoneinstitute.ca/news/practice-ready-ontario-applications… and https://www.cbc.ca/news/canada/new-brunswick/doctors-college-physicians…
- 22 For further details, see https://novascotia.ca/news/release/?id=20230321001
- 23 For further details, see https://news.ontario.ca/en/release/1004479/ontario-helping-family-docto…
- 24 For further details, see https://www.cihi.ca/en/health-workforce-in-canada-in-focus-including-nu… and Aggarwal et al. (2023).
- 25 Last year, British Columbia developed a new longitudinal capitation payment model, accounting for the number and complexity of patients, the time of direct care, and administrative costs. Such a mechanism can prevent family physicians from avoiding the sickest patients and likely attract physicians to practice family medicine. However, this model needs to be evaluated to see its effectiveness on patient care.
- 26 Shadow billing refers to a process where physicians under alternate payment models submit specific claims for medical services provided to patients that result in no payment. This allows the provincial Ministry of Health to track healthcare service delivery. Shadow billed claims are either not paid at all or paid at a lower percentage of the FFS rate (depending on the physician’s agreement). While shadow billing can add administrative burden, keeping track of services provided to patients helps monitoring and evaluation. Governments can explore opportunities for digital solutions such as auto-fill to automate the billing process.
- 27 In Ontario, after hours care is required for all models except comprehensive care model and NP-led clinics. However, to my knowledge, there are no regulations in place to enforce after-hours care, nor have there been evaluations of the effectiveness of this requirement on patient access. For instance, a report by OAGO (2016) revealed that in 2014/15, 60 percent of Family Health Organizations and 36 percent of Family Health Groups did not work the number of weeknight or weekend hours required by the Ministry.
- 28 For further details, see https://www.cihi.ca/en/nurse-practitioners#:~:text=In%202022%2C,growth%….
- 29 While NPs can independently treat and diagnose patients, hospitals or family physician-led clinics sometimes treat them as assistants. The overlap of services provided by nurse practitioners and family doctors can create tension between the professions. There needs to be an organizational change where nurse practitioners work independently from physicians more often (Drummond et al. 2023).
- 30 The model is expected to include payment for a specified number of clinical hours and other commitments, such as caring for a certain number of patients. For further details, see https://open.alberta.ca/publications/nurse-practitioner-primary-care-pr…
- 31 For further details, see https://globalnews.ca/news/9479016/demand-high-pharmacy-primary-care-cl…
- 32 For further details, see https://news.ontario.ca/en/release/1003584/even-more-convenient-care-cl… and https://www.bcbudget.gov.bc.ca/2023/default.htm
- 33 Kiran et al. (2022b) find that approximately one-fifth of patients receive team-based primary care as part of a Family Health Team whereby physicians formally enroll patients, are paid via blended capitation, and have mandatory after-hours care.
- 34 The top five providers are nurse practitioners, nurses, pharmacists, psychologists, and psychotherapists. For more details, see question 46 at https://data.ourcare.ca/all-questions
- 35 In 2016, Ontario’s Auditor-General found that the average family physician working in a Family Health Organization was working just 3.4 days a week, despite being paid for a full week.
- 36 In Newfoundland and Labrador, patients registered on Patient Connect will have access to a virtual physician available Monday to Friday 9 am to 8 pm.
- 37 For further details, see https://www.princeedwardisland.ca/en/service/virtual-health-care-for-is…
- 38 For further details, see https://www.nshealth.ca/clinics-programs-and-services/virtual-care-ns






