The Study in Brief
- The intense debate pitting private versus public healthcare in Canada needs a reality check. Private aspects of healthcare exist in different forms and to varying degrees across Canadian provinces, largely depending on their respective legislation and regulations.
- For healthcare professionals providing insured services, most bill through the public system, but not all. The current and future scope of their role is the pressing issue at hand.
- Health Canada has had success in eliminating extra billing and user fees under sections 18 and 19 of the Canada Health Act. However, provinces have considerable authority in determining key terms like “medically necessary” or “insured services” that are covered under the Act. The result has been a diversity of approaches.
- Provinces have the legislative tools to constrain the growth of private healthcare, if that is their objective. Similarly, provinces have considerable authority to increase the scope of private healthcare, if that is their objective (even within the current parameters of the CHA), by revising provincial legislation or regulation.
- Either way, the specific policy direction undertaken would be different for each jurisdiction, as the legislative and other barriers to private healthcare (such as market size limiting the viability of private delivery) vary across provinces. This Commentary provides clarity about the different forms of "private" healthcare and a comprehensive view of the current policy landscape defining the balance between public and private healthcare.
Special thanks to Bill Lahey, for his extraordinarily encyclopedic comprehension of health law and provincial statutes; to Katie Booth, Sara Allin, and Raisa Deber, for commenting on previous drafts; to DoctorsNS, for allowing me to test drive an early version on an intimidatingly large number of physicians; to the provincial insurers and regulatory colleges I contacted, for listening patiently to my arcane queries and for finding the right person to answer them; and to the numerous reviewers whose insights were exceptionally helpful. They include Rosalie Wyonch, Benjamin Dachis, Duncan Munn, William Robson, Åke Blomqvist, Tim Brennan, Neil Fraser, Mike Hamilton, Geneviève Lavertu and anonymous reviewers. The author retains responsibility for any errors and the views expressed.
Introduction
All health systems incorporate some mix of public and private healthcare. In 2021, public sector spending in Canada amounted to 73 percent of total healthcare expenditure, exactly equivalent to the OECD average of 73 percent (OECD 2023). Yet these summary figures tell us little about the public/private contours of any healthcare system. Private healthcare can manifest in a multitude of ways, and the precise configuration of the relationship between public and private healthcare tells us more about the system than the absolute level of public or private spending.
Under the Canadian Constitution, provinces have wide-ranging jurisdiction over the provision of healthcare in Canada, both explicitly (hospitals) and through judicial interpretation (“matters of a merely local or private nature,” as well as authority over insurance). The Canada Health Act (CHA) does provide a national framework (supported by federal transfer funds) that has, for several decades, ensured a certain level of congruence across provinces in the provision of public healthcare. But each province’s health legislation is unique, and it is this interplay between federal and provincial legislation that provides a regulatory space for private healthcare. Variation across provinces means private healthcare in Canada is not a uniform phenomenon.
The objectives of this Commentary are fourfold: first, to describe the ways we can understand “private” healthcare; second, to explain the different ways provincial legislation permits or prohibits aspects of private healthcare; third, to discuss the supply- and demand-side variables causing private healthcare to take its current shape across provinces; and fourth, to analyze the relationship between provincial healthcare legislation and the CHA with reference to the expansion of private healthcare in Canada. This Commentary does not address the utility of private healthcare per se. Rather, it focuses on the confusion inherent in so many discussions referencing “private healthcare.” Both exponents and critics of private healthcare can pick and choose from numerous manifestations of private healthcare to support their respective positions. By requiring proponents and opponents to clarify precisely what they mean by “private healthcare,” the potential costs and benefits can be more clearly identified in each case.
What Do We Mean by “Private Healthcare”?
Critics of private healthcare point to the costs and inequities of the American healthcare system to argue against it, while proponents reference European mixed public/private models to show how effective it can be. Any discussion of the role of private healthcare should therefore first clarify what, precisely, is meant by “private healthcare.” Healthcare systems can generally be broken down into three constituent parts: delivery, financing, and regulation. Any of these elements can include a public or private (for-profit or not-for-profit) component (Wendt et al. 2009; Böhm et al. 2013; Marchildon 2022).
Delivery of Healthcare Services
Much healthcare in Canada is delivered by private providers. When medicare was introduced in Saskatchewan in 1947, physicians vehemently protested. A settlement was reached only when the province agreed to recognize physicians as private independent operators rather than as employees of the state (Marchildon 2020). This model was followed by other provinces as they introduced their own medicare legislation. Ambulance services across Canada are often private, with these companies negotiating service contracts with health authorities or provinces. Nursing care in hospitals and district nursing programs is generally provided publicly, but private nursing firms (such as the not-for-profit VON for home care, or for-profit firms supplying temporary placements in hospitals) are also commonly utilized.
Historically, hospitals in Canada (especially those founded by religious orders) were largely based on a private, independent, not-for-profit model. As hospitals became amalgamated into health authorities, they were consolidated in provincial governments’ financial statements and their operation was generally subsumed within the public infrastructure – even as many (especially larger) hospitals with boards of directors remain not-for-profit organizations.
What, exactly, is a “not-for-profit” (NFP) organization in Canada, and how does it differ from a private or a public one? Legally, NFPs are “bodies corporate without share capital”: in other words, revenues must be directed to the mission of the organization rather than to shareholders. NFPs also enjoy specific tax breaks. Unlike fully public bodies, however, they are self-governing. Generally, they will have boards of directors who are accountable for funds raised and debts incurred. Like directors in a private company, these directors have a fiduciary responsibility to use resources wisely. Unlike private companies, directors of NFP organizations are directly responsible to the corporate entity rather than to members (i.e., shareholders). The corporate entity, in turn, is responsible to the government jurisdiction (federal or provincial) wherein it is incorporated.
Increased attention has been paid to private surgical companies. Individual medical specialists are generally considered independent private operators who contract their services to medical facilities or universities, although their payment models often include elements such as base salary, research stipend, fee for service, etc. Surgical specialists have in many provinces established discrete private businesses where bulk services (a specific number of certain surgical services) are provided over a set period for a negotiated price (e.g., the Shouldice Hernia Centre in Ontario or Scotia Surgery in Nova Scotia). They may use public infrastructure (hospital operating rooms) or provide their own physical space. There is considerable debate whether contracting these services is superior to establishing them as part of the public system (e.g., Day 2023; Lewis 2022; Longhurst 2023). However, as the funding and administration of these services is controlled by provinces (or provincial health authorities), and as patients use these services as they would fully public services (i.e., free at point of delivery), they are not considered a “two tier” form of access to healthcare. Patients cannot access these services directly; rather, they are routed through the public system. Grey areas of private service delivery, described in more detail below, include the private delivery of medically necessary diagnostic services, infusion clinics on hospital sites, and certain forms of virtual care.
Also relevant to the discussion of private delivery is the type of private entity under consideration. “Private” hospitals that are not-for-profit may in fact operate more like a public institution than a private one; here one might usefully distinguish institutions which are functionally embedded in provincial healthcare system (e.g., via accounting practices) from those that operate at arm’s length. Conversely, evidence from the United States suggests private not-for-profit hospitals can also show the kind of profit-driven behaviour more commonly seen in for-profit entities (Silver-Greenberg and Thomas 2022). Others have argued that small independent private health clinics (such as Algomed or Bluenose, in Canada) are in a different category from large American corporate entities (such as the Hospital Corporation of America) (Deber 2003).
Financing of Healthcare Goods and Services
As noted, some privately provided services (such as ambulance services or surgical clinics) are often funded publicly. And, while it is not as common, publicly provided services can be funded privately (e.g., in systems where money follows the patient, private insurers may be able to find places for their patients in publicly funded hospitals). Charitable NFP organizations can be another source of healthcare funding. In Canada, much attention is paid to the division of healthcare into services that are, or are not, insured publicly. For example, the provision of cosmetic surgery (undertaken for aesthetic reasons) is commonly private, and is paid for privately and directly out-of-pocket. The private provision of services that are publicly funded (such as cataract or hip replacement surgery), as noted, is more controversial, but is not uncommon within Canada. The main point of controversy in Canada is whether publicly insured services should also be available for direct purchase to individuals within the private sector, bypassing the public system altogether.
Out-of-pocket financing in Canada is largely targeted to healthcare services that are not covered by public insurance (the precise list of insured versus non-insured services varies across provinces). Only 12.6 percent of Canadian healthcare expenditure in 2021 was comprised of out-of-pocket spending (WHO 2023); the remainder was covered by public or private insurance.
So how is healthcare insurance structured in Canada?
Public insurance: In all provinces, most medically necessary healthcare services are largely funded on a tax-based model, where citizens support healthcare services through their general tax contributions. Some provinces do require provincial inhabitants to pay “healthcare premiums” but, as these contributions simply go into the provinces’ general operating funds, rather than a bespoke account used only for healthcare, these premiums can be considered simply as another form of taxation. As a condition of receiving federal health transfers, the CHA requires that each province has a public insurer. Böhm et al. (2013) argue, for this reason, that states such as Canada and Australia, which are structured on a public insurance system, are more properly considered to possess “national health insurance systems” rather than “national health systems,” as typified by the UK.
Each province has the authority to determine what it insures publicly (which is why coverage for “medically necessary services” varies across provinces). In general, medically necessary services provided by physicians and in hospitals are covered (as required by the CHA) but, as explained below, this is much more complicated than it appears. Services such as vision care and dental care provided in hospitals are also generally covered, as are diagnostics, physiotherapy, and other related services.
Provinces are not required to cover everyone: those in the armed forces or federal penitentiaries, for example, are insured by the Government of Canada. Although provincial healthcare systems provide many of the services for these specific groups, the provinces are reimbursed by the federal government. Those injured in the workplace are usually covered by workers’ compensation. Certain categories of migrants (such as refugees) are also insured federally until they receive permanent citizenship status, whereupon they fall under provincial insurance. Depending on the type of work and the length of stay, migrant workers are insured both through provincial health plans and workers’ compensation programs (for a fuller discussion, see Fierlbeck and Marchildon 2023).
Most provinces expand public health insurance beyond what is required by the CHA. While the CHA does not specifically mandate the public provision of dental care, optometry services, and pharmaceuticals outside of hospitals, provinces generally have some form of coverage of these services for vulnerable groups. These are determined either by cohort (e.g., seniors or children), service (pharmacare or dental care), income category (below a certain ceiling), or some combination of all three. These programs vary considerably across provinces.
Private health insurance: Formally, there are several types of private health insurance, each serving a different function.
- Supplementary health insurance covers any goods or services that are not covered by public insurance. In Canada, these include companies like Blue Cross, Sun Life, or Canada Life Assurance. Any healthcare system incorporating public insurance will also have an array of private and private not-for profit supplementary health insurance companies which generally cover vision care, physiotherapy, pharmaceuticals, travel insurance, etc.
- Complementary health insurance completes the cost of a service, where public or social insurance only pays partial costs. In many countries, for example, public insurance will only cover around 60 percent – 80 percent of hospital stays, pharmaceuticals, primary care, and sometimes even emergency care. In these cases, private insurance will “top up” the remaining costs so patients do not have to pay out-of-pocket. Some insurers may ask patients to pay the remaining costs up front, and reimburse them after the fact; others may cover the costs at point of payment. This “top up” system is not common in Canada, but in Quebec (which mandates pharmacare insurance) private insurers are allowed to cover any co-pays for pharmaceuticals that patients must pay directly for amounts not covered by the mandated insurers.
- Substitutive health insurance applies in systems (e.g., in Germany) where citizens earning above a set income are allowed to opt out of public insurance systems altogether, and use private for-profit insurance to cover medical needs.
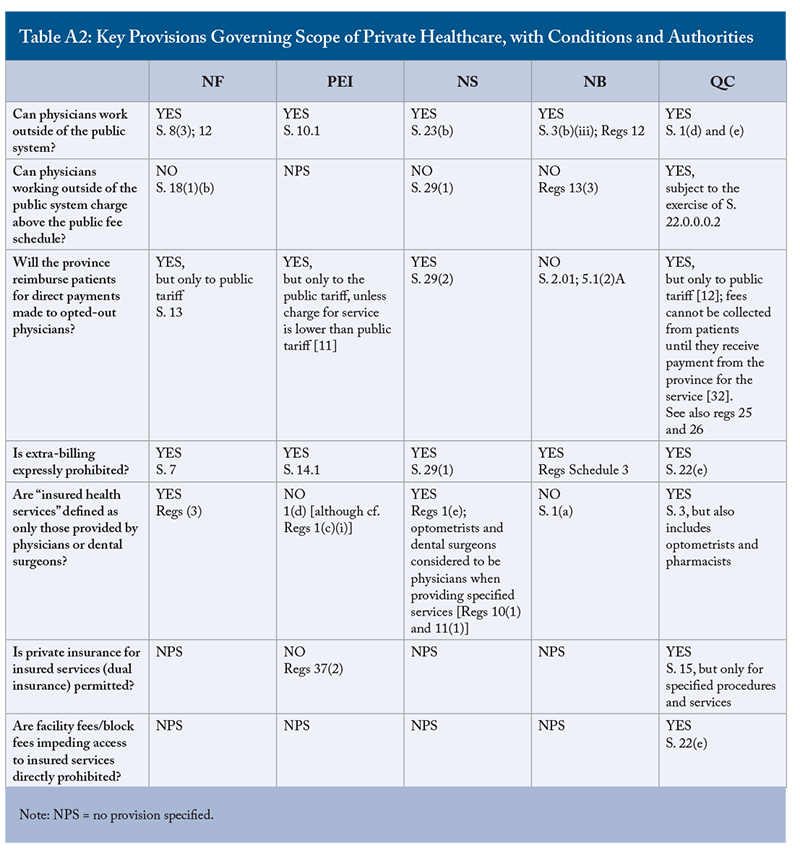
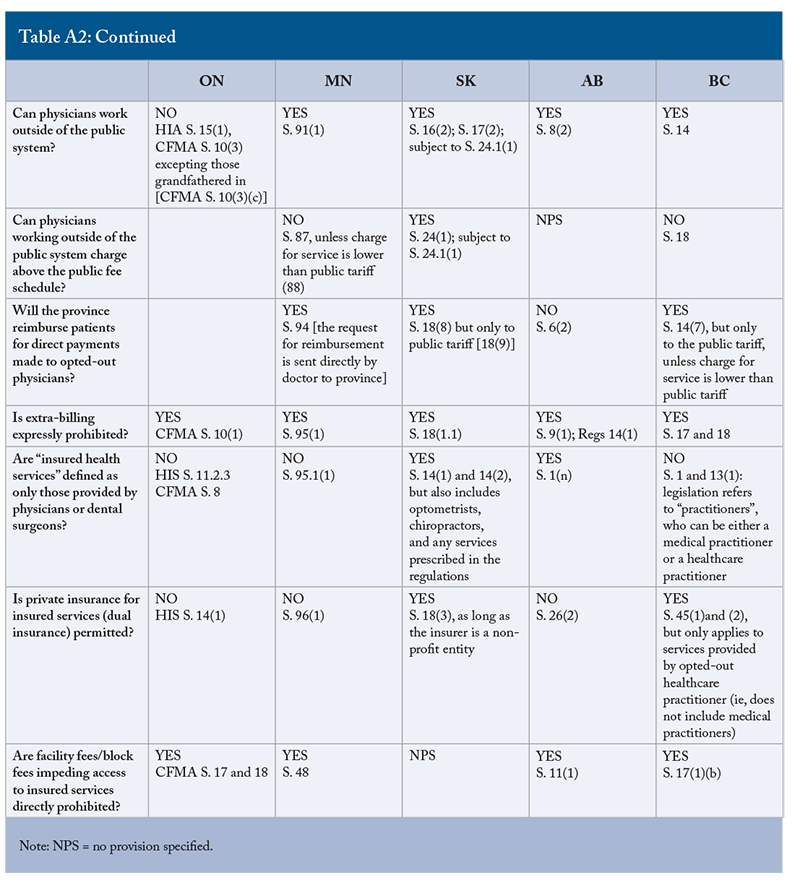
- Duplicative (or “dual” or “parallel”) health insurance is the source of most political controversy in Canada. Duplicative insurance privately covers services that are also offered in the public sector. Four provinces (Ontario, Manitoba, Alberta, and PEI) explicitly prohibit duplicative insurance, three (Saskatchewan, British Columbia, and Quebec) explicitly permit duplicative insurance under certain conditions (i.e., only for certain services, only if the insurer is private not-for-profit, only for services provided by practitioners outside of the public system), and three (Newfoundland, Nova Scotia, and New Brunswick) neither expressly permit nor prohibit it (Appendix Table A2).
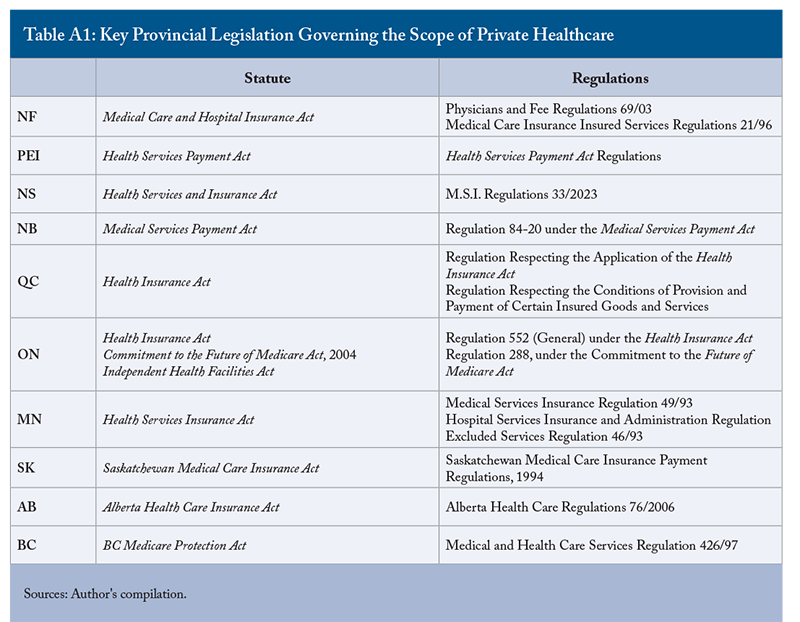
Tables A1 and A2 appear following the references section at the end of the document. The advantage for those with duplicative insurance is that they can access these services quicker, or access more enhanced variants of these services. It is really with this particular kind of private insurance that the issue of “two tier” healthcare arises. The argument in favour of duplicative insurance is that it “takes pressure” off of the public system (e.g., Globerman 2020), while other research has found that public wait times actually increase when publicly insured services become privately available. One reason given for this is the depletion of resources from the public sector. Policy analysts also suggest that those offering private services have incentives to keep public wait times longer, as patients will only find private services attractive if they cannot easily access them in the public sector (e.g., Besley et al. 1998; Duckett 2005). Countries such as the UK that permit duplicative insurance nonetheless continue to have considerable issues with long wait lists in the public health system (e.g., Duncan et al. 2023).
- Private not-for-profit insurance: Another category of health insurance that causes much confusion is statutory health insurance (SHI; also referred to as “social health insurance” or the “Bismarck health system”). This system is quite common in Europe, although the precise configuration varies across states. In this model, health insurance is not covered in the first instance through general taxation revenue. Rather, workers and employers pay into “sickness funds,” which provide health insurance benefits depending on the terms negotiated. These sickness funds are technically “private” bodies operating on a not-for-profit basis. They are, however, highly regulated in their authority and function. Because of the degree of regulation – and the importance of the social function they fulfill – they are generally considered a form of “public” insurance. However, governments tend to differ in their approach to consolidating these operations into government expenditures.
This is similar to the categorization of workers’ compensation in Canada where a highly-regulated, not-for-profit form of health insurance is generally considered to be within the “public” category of health expenditure. Jurisdictions using this model of health insurance have different methods for covering unemployed or retired persons, often including funds directed from government taxation revenue or from pooled sickness funds.
Regulation of Healthcare Financing and Delivery
The nature of “private” healthcare is determined not only according to the way services are delivered or funded but, more importantly, according to the way they are regulated. Permitting a “private” form of health service or insurance is not an all-or-nothing condition; governments have the authority to determine the terms and conditions under which these services are to be offered. There can, for example, be limitations on the kinds of services offered or insured, on the professions allowed to offer them, on the prices that can be set for them, where they can be provided, and so on. These limits, as discussed below, can be enough to discourage the provision of health services even when these services are technically legal, as the terms within which private services are allowed may not be sufficiently profitable. In the European Union (EU), governments are more restricted in their ability to regulate private healthcare services because, ultimately, the ethos of the EU is to maintain the free movement of goods and services. Fully public health services are under the authority of member states but, where states utilize private components in their healthcare systems, attempts to limit the ability of private health firms to compete can result in charges of breaching fair-competition regulations. In Canada, however, there are fewer restrictions on the limits that provinces can place on private health providers, given the political will to do so. The regulatory aspects of healthcare financing and delivery will be addressed in more detail in the next section.
Another category of “private” healthcare is the implementation of private-public partnerships (P3s) in healthcare (McKee et al. 2006). In the past, this has been limited to large capital projects, such as the construction of hospitals, but more recently the implementation of P3s has expanded to the point where verdicts on their effectiveness can be rendered. Importantly, there is no single model of public-private partnerships; each is generally negotiated on its own terms. Proponents explain the logic of this approach as capturing the advantages of both systems: governments can access more competitive financing for projects, while firms undertake the process of construction more efficiently with each day of overrun increasing the cost of a project. Critics argue that the logic of P3s rests in the effectiveness of offloading costs to the other partner, and that the party with the most expertise in negotiating P3 contracts (generally large multinational firms with experience in this area) are those who are most able to shift costs. At the same time, because P3 projects allow costs to be diffused over a long period of time, budget-conscious governments have been eager to enter into these agreements.
Empirical evidence suggests that the effectiveness of P3 projects in Canada has been quite varied (Murphy 2008; Vining and Boardman 2008; Siemiatycki 2015). More recently, provinces have expanded the use of P3s to include large outlays for medical infrastructure. These agreements, often known as “value partnerships” or “managed equipment service agreements,” generally focus on diagnostic equipment – providing MRIs, CT scans, and X-rays – and they range from 15 to 30 years. The private partner will source, install, and maintain this equipment over the life of the agreement. As the private partner owns the equipment and covers the cost of installation, there are minimal upfront costs for the public partner. Other advantages of this model include a reduction in equipment downtime, decreased administrative burden in monitoring equipment maintenance, protection from unpredictable costs involved in equipment failure (CADTH 2022), and a replacement plan for equipment that reaches the end of its recommended useful life. At the same time, long-term service contracts can diminish flexibility in accessing different equipment over the lifespan of the contract, and the private contractor may demand confidentiality agreements which could diminish the transparency and accountability of the process. Like other forms of P3s, the effectiveness of managed equipment services will largely depend on the specifics of negotiated agreements, including clearly defined outcomes and expectations, as well as transparent and accountable protocols and public scrutiny of this documentation (CADTH 2022).
While “internal markets” are not formally an aspect of private healthcare per se, they frequently arise in discussions of the utility of private healthcare mechanisms in the reform of public healthcare. Most famously employed in the Thatcherite reforms of the National Health Service in the United Kingdom, this model simply divides public healthcare professionals into “purchasers” of acute care services (usually primary care professionals) and “providers” of acute care services (usually hospitals). The theory underlying the purchase-provider split is that GPs will select the best value for money, obliging hospitals to compete by offering quality services for less. While the results of Britain’s experiment with the internal market are mixed at best (for a discussion of the internal market reforms see, e.g., LeGrand, Mays, and Mulligan 1998; and Ham 2007), a number of other countries (such as the Netherlands) have since incorporated this mechanism into their own healthcare systems.
Private Healthcare within the Context of Provincial Legislation in Canada
The scope for private healthcare varies considerably across Canada. It is shaped by the provincial legislation governing healthcare services and insurance. A key issue is the extent to which publicly insured services can be accessed privately and directly. For non-insured services (such as cosmetic surgery), regulation can be quite minimal, essentially falling under the purview of the medical Colleges for the respective healthcare professions. Insured services provided directly to patients outside the sphere of public insurance, and the regulation of private insurance covering these services, are subject to an array of regulatory mechanisms. Generally, the more healthcare systems incorporate parallel private financing, the more prevalent and restrictive these regulations are. The regulatory regimes surrounding the provision of parallel private financing in both Australia and Ireland, for example, illustrate this tendency for a more “open market” in health services to require a more robust regulatory framework (Hurley 2020). Somewhat paradoxically, greater privatization of healthcare also requires much more government engagement in setting parameters, including the capacity to monitor and enforce regulations.
In 2001, Flood and Archibald outlined the ways regulatory mechanisms were utilized by provincial governments to limit the scope of duplicative healthcare in Canada. While the gradual evolution of provincial legislation has meant that the empirical results of the study are no longer current, the categorization of these mechanisms remains insightful.
Prohibition from Practicing Outside of The Public Healthcare System
The most effective, but least utilized, regulatory instrument restricting the provision of private healthcare is the prohibition against physicians opting out of the public insurance system. In Canada, this provision only applies in Ontario, where section 3 of the 2004 Commitment to the Future of Medicare Act explicitly prohibits physicians or “designated providers” from accepting payment other than from OHIP or other designated public authorities for insured services (excepting physicians who were given grandfathered status within the Act).
Constraints on Physicians Allowed to Work Outside of The Public System
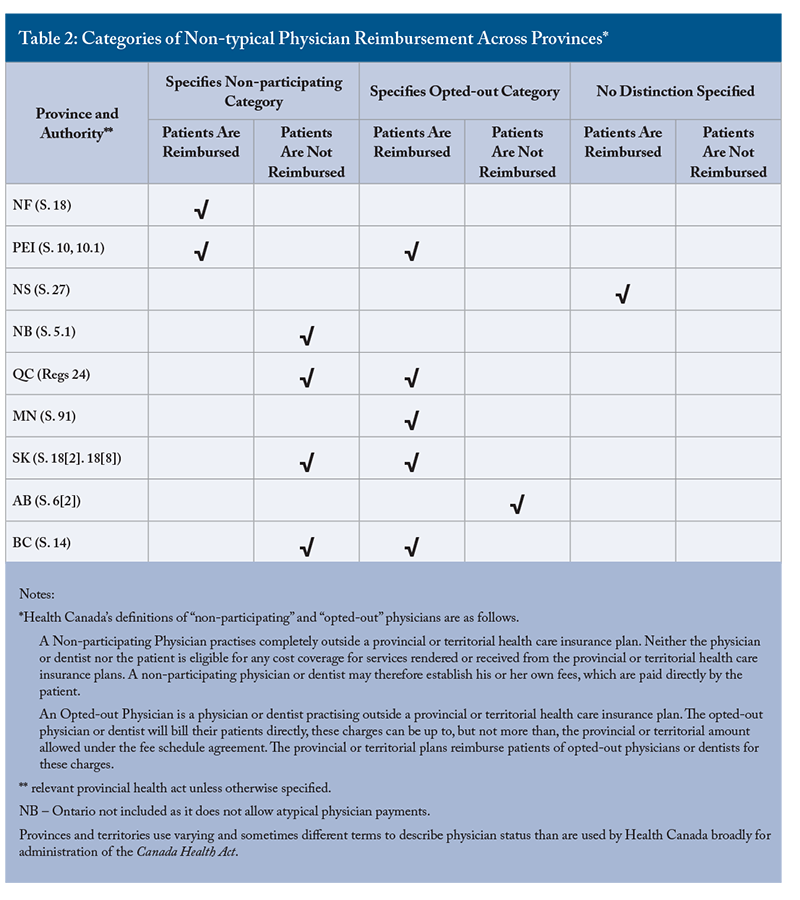
For physicians permitted to work outside the public system, there are two separate but related provisions: 1) physicians may bill patients directly, and those patients may be reimbursed by the province, but billing fees are limited to the fee schedule set out in the public system; or 2) they may bill patients directly at fee levels not limited by the public tariff, but these costs will not be reimbursed. Importantly, Health Canada distinguishes between “non-participating” and “opted-out” physicians (Health Canada 2019). A “non-participating” physician, according to Health Canada, practices completely outside a provincial or territorial healthcare insurance plan. Neither physician nor patient can receive payment or reimbursement from public insurance plans; consequently, physicians can set their own fees, and receive payment directly from patients. In contrast, while Health Canada deems an “opted-out” physician also to be one “practicing outside a provincial or territorial health insurance plan” (Health Canada 2019), opted-out physicians are informally considered to be working within the public system to the extent that they are subject to its terms. Specifically, Health Canada considers opted-out physicians to be those who can bill their patients directly (up to the fee set by the public fee schedule). In turn, the province will reimburse patients of opted-out physicians if claims are submitted to it. As we shall see below, however, this distinction is not as clear in practice as it might seem on paper.
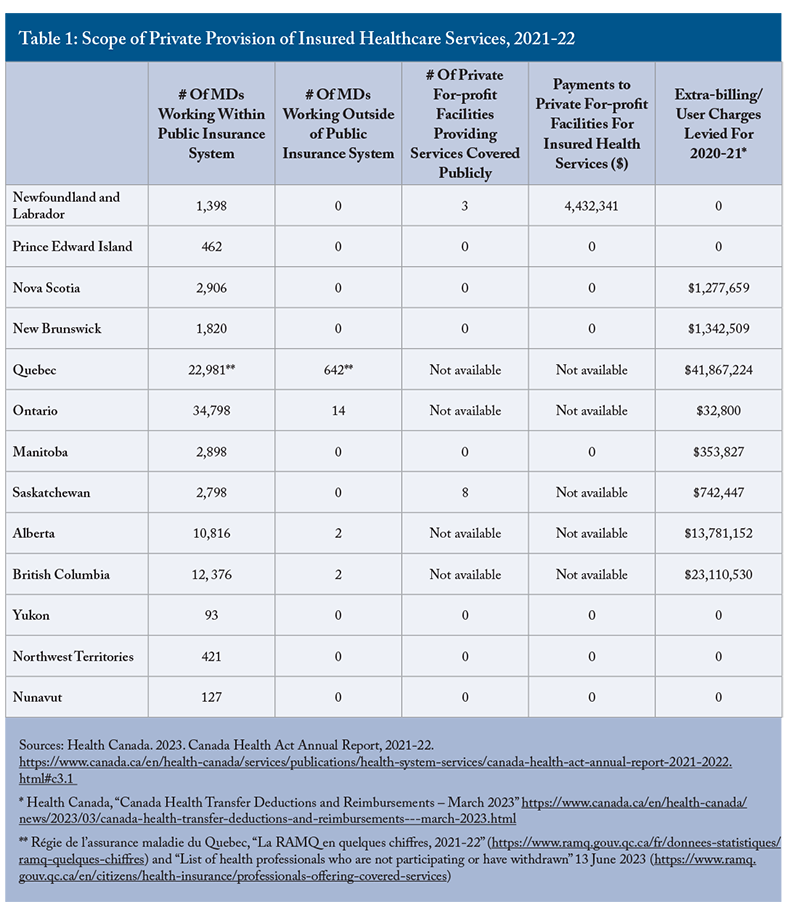
Of the nine provinces permitting physicians to leave the public insurance system, all of them (excepting New Brunswick and Alberta) will reimburse patients the cost of insured services provided privately. None will reimburse costs above the amount set by the public fee schedule, and some specify that, if the actual cost incurred is lower, that will be the cost reimbursed. In general, patients will seek reimbursement from the province by submitting the receipt for services to the provincial insurer; in Manitoba, however, the claim request must come from the treating physician. Notably, however, Newfoundland, Nova Scotia, New Brunswick, Prince Edward Island, Manitoba, and Saskatchewan currently have no physicians working outside of the public system (Table 1), and so this measure costs these provinces very little, either financially or politically.
In effect, both requirements can limit the scope for private healthcare. If fees remain the same within and without the public system, physicians have no financial incentive to leave the public system. If higher fees are allowed only if patients are not reimbursed, then patients have no incentive to seek a non-participating physician as long as they can receive the same services free at the point of delivery in a timely manner.
Prohibition Against User Fees and Extra-billing
Sections 18 and 19 of the CHA require provinces to prevent both user fees and extra-billing as conditions for receiving federal health transfers. Because the federal government has, over time, clawed back these funds in provinces where user fees and extra-billing have occurred, provinces have gradually revised provincial statutes to assert an explicit proscription against them. In this way, physicians working within the public insurance system cannot levy fees directly on patients above what is set by the public fee schedule.
Prohibition on Facility Fees and Restrictions on Block Fees
In 1995, Ottawa announced a new policy clarifying the federal position on private clinics. Specifically, the “Marleau Letter” stipulated that, under the terms of the CHA, patients should not be charged “facility” fees: i.e., charges covering the costs of the facility above and beyond physician fees for services provided. Provinces insuring services provided by physicians in a private clinic must also cover all relevant facility fees or face a deduction in federal health transfers. Some provinces (including Ontario, Manitoba, Alberta, and British Columbia) expressly prohibit these fees. Smaller provinces generally do not reference facility fees in their legislation, likely because private clinics per se have not been prevalent in these provinces.
“Block” fees, in contrast, are (usually annual) fees charged by clinics which may provide a combination of insured and uninsured services. Some provinces stipulate that, where a private clinic provides a mix of insured and uninsured services, these annual “block” fees cannot obstruct access, or provide preferential access, to the insured services. Ensuring compliance with this provision may, however, be rather difficult.
The prohibition on dual insurance is especially prevalent in larger provinces (such as Ontario and British Columbia) where a critical mass of population and higher incomes make private insurance more economically feasible. As Hurley (2020) explains, the viability of a private insurance industry depends on having a market large enough to attract a sufficient number of relatively healthy people and avoid adverse risk selection. It is noteworthy that those provinces permitting a duplicative private insurance stream without specific conditions or categories involved (Newfoundland, Nova Scotia, New Brunswick, and Saskatchewan) are small provinces where the private insurance market has shown no interest in covering insured health services. Quebec is an interesting case here, as it has a partial ban on private health insurance. This is a result of the Chaoulli constitutional challenge, culminating in 2005, that required Quebec to allow private health insurance for services with substantial wait times (hip, knee, and cataract surgery). However, Quebec countered this requirement by channeling considerable funding into reducing wait times for these services, thus removing the economic incentive for individuals to seek private insurance. By 2020, Quesnel-Vallée et al. were able to report that “duplicative health insurance did not develop at all in Quebec with regard to the list of approved services.” The ban on duplicative private insurance in British Columbia was also targeted in the Cambie constitutional challenge that culminated in 2020 with an unsuccessful verdict.
The measures noted above do not exhaust the possible ways private healthcare can manifest itself, or the ways in which provinces can influence the level of private healthcare in Canada. As Thomas (2020) suggests, for example, a province could use exclusivity clauses in physician contracts, impose income limits on dual practice physicians, or incentivize physicians to remain solely in the public sector by offering specific financial bonuses or promotion. These regulatory options were of particular interest when it was unclear what the outcome of the Cambie case would be. However, with the resolution of Cambie supporting the authority of provinces to impose regulatory limits on private care, and with the refusal of the Supreme Court of Canada to hear an appeal in this matter, the discussion regarding alternative forms of private regulation has waned. Even so, the significant operational strains currently evident in the public healthcare system suggest that political pressure for increased access to privately provided, publicly insured services will continue to increase. “Grey” services, such as private healthcare navigators who expedite access to public services, are also increasingly common.
Disruption and the Dynamics of Private Healthcare Regulation in Canada
Regulatory mechanisms are by nature stable and long-lasting. Whether they work depends not only on how well they are drafted, but also on the relative constancy of the social and political conditions they address. In the case of provincial healthcare, the nature of healthcare provision (and arguably healthcare itself) has changed dramatically in recent years. The sudden and intense pressures imposed by the COVID-19 pandemic did affect healthcare provision significantly, but these trends were quite visible well before COVID-19 emerged, and in fact only intensified as the pandemic ebbed.
Many of these pressures are human-resource oriented. One key indicator is access to primary care providers, which has decreased considerably in a matter of years. According to Nova Scotia’s registry dashboard, for example, almost 15 percent of the population as of June 1, 2023, did not have access to a stable primary healthcare provider, almost double compared to the previous year (Nova Scotia Health 2022). In British Columbia, 23 percent of the population in 2022 did not have a primary care provider (Angus Reid Institute 2022). Even those formally listed with a primary care provider have problems accessing primary care services: 60 percent of respondents across the country experienced “strained” or “difficult” access to non-emergency care. Wait times for emergency services and elective surgeries are also a matter of public concern. (Angus Reid Institute 2022).
The pressures currently experienced in healthcare systems have various causes and have manifested various effects. Underlying it all, however, is the expanding nature of healthcare itself. We have more treatments with more clinical options than ever before. This is a positive advance but, at the same time, it is a more intensive treatment context: more potential diagnostic tests available, for example, means more tests to be ordered and reviewed; while more drugs available means more meetings between patients and healthcare providers to monitor effectiveness, and to assess the best choice for each person. One study, tracking changes in primary care physician workloads between 1996 and 2018, found increases of 36.1 percent in time spent addressing lab tests alone, and an increase of 55 percent in time spent with emergency department follow-ups (Lavergne et al. 2022). A wider selection of pharmaceutical products also increases instances of adverse reactions and interactions, especially in older adults who tend to be prescribed multiple drugs. The Canadian population itself is aging overall, which again means a larger proportion of the population requiring more complex care.
At the same time, the profile of healthcare providers is itself changing: physicians are now more likely to be female, and to have partners with demanding full-time jobs. Younger physicians are also concerned with work-life balance issues. These factors mean that physicians tend now, as a profession, to work slightly fewer hours per week than in the past (CMA 2023). Of the hours worked, an increasing number are spent uploading data to electronic platforms (see, e.g., DoctorsNS 2023).
In the past decade, three trends have been particularly notable in changing the way healthcare has been provided.
Services Provided Outside of the Context of Hospital Care
The first trend addresses the scope of services that can be provided outside the context of hospital care. This is a particularly Canadian issue, as it is informed by the CHA (and its predecessor legislation, the 1957 Hospital Insurance and Diagnostic Services Act and the 1966 Medical Care Act), which stipulates that provinces must insure all insured health services provided by hospitals as a condition of receiving federal funding. Cost-sharing medical services provided only in hospitals created incentives for provinces to provide more healthcare services in hospitals rather than in the community, even as this made them more expensive and less accessible. At the same time, cost-sharing primary services provided only by physicians meant that other healthcare professionals doing some of the same tasks as GPs (such as psychologists, nurse practitioners, or practice nurses) were often not utilized. In 1977, the terms of federal transfers were renegotiated to permit provinces more scope to self-fund services that fell outside of hospitals (such as long-term care). Provinces did not, however, take advantage of this measure (Naylor et al. 2020).
Some services, in particular diagnostic ones, have increasingly been provided outside of hospitals. These off-site facilities were understood to fall outside of the CHA and could therefore be offered within the private sector (as Quebec has maintained: see Quesnel-Vallée et al. 2020). Because of this, Ottawa introduced the Diagnostic Services Policy in 2018 which stipulated that diagnostic services considered medically necessary were to be publicly insured, regardless of whether they were provided in public or private facilities (Health Canada 2023a). In spite of this clarification, in December 2022 Ottawa issued a statement declaring that many provinces were continuing to permit private facilities to charge for medically necessary diagnostic tests. This practice, stated the federal Minister of Health, Jean-Yves Duclos, was “not acceptable, and will not be tolerated” (Health Canada 2023b). Subsequently, Health Canada levied deductions against Quebec ($41,867,224), British Columbia ($17,165,309), Alberta ($13,781,152), New Brunswick and Nova Scotia ($1,277,659 each), Saskatchewan ($742,447), and Manitoba ($353,827) for diagnostic services alone (Health Canada 2023c). To date there has been no indication that these fines have led provinces to take action on diagnostic facilities in their provinces.
A second, more recent trend has been the utilization of virtual technology (phone, text, or video consultations). In 2016, Akira and Dialogue began offering virtual healthcare services to large private corporations; by 2018, Maple was offering private online services directly to Canadians. But it was the COVID-19 pandemic which solidified the trend in virtual care, as provincial governments introduced fee codes for remote medical consultations (Fierlbeck and Marchildon 2023). Initially established during the pandemic for patients who could not access in-person services, provincial governments contracted with private virtual health providers such as Telus or Maple to provide “virtual walk-in clinics” for patients. Post-pandemic, jurisdictions continued with these services to meet the growing waves of patients without primary care providers. By the end of 2022, the utilization of Maple’s virtual services was 90 percent higher than it had been prior to the pandemic (Frangou 2023). As these services were publicly insured, they were free at point of access for patients, but the limited funding of these services provided by provinces meant that many people found it difficult to access these appointments, which tended to fill up quite quickly. Ontario, in December 2022, reduced the fees physicians could claim for virtual services, also resulting in lower numbers of publicly insured virtual consultations available. At the same time, these virtual healthcare companies maintained – or even expanded – their privately-available healthcare services, so that patients who had become accustomed to using the publicly funded virtual services were primed to pay privately for them if they remained unable to access publicly funded services.
Many primary-care clinics continue to offer online consultations which tend to be popular with both providers and patients. The regulatory framework is complex, as public insurers must determine whether providers should be resident in the province where they provide services and, if not, whether they must at least be licensed in that province. These provisions vary across provinces. Private for-profit virtual-care services have an even more complex regulatory context. As patients can access services beyond provincial borders, any provincial restrictions on the provision of private care become difficult to monitor and enforce. It also raises the question of the degree to which private providers can, or should, be able to facilitate patients’ access to the public system through ordering diagnostic tests or consultations. Canadians can also access clinical-care apps situated outside the country, which means that physicians providing medical advice are even further beyond the reach of professional regulatory colleges. Furthermore, there is the possibility that for-profit virtual care providers could engage in data-mining disaggregated healthcare information supplied by clients, and sell it to third parties (Frangou 2023).
In March 2023, then Minister Duclos sent a letter to his provincial and territorial colleagues expressing concerns regarding charges for virtual healthcare services, indicating his “intention to clarify in a separate Canada Health Act interpretation letter that, no matter where in the country Canadians live or how they receive medically necessary care, they must be able to access these services without having to pay out of pocket” (Health Canada 2023e). In July 2023, Mark Holland replaced Jean-Yves Duclos as Minister of Health, and the status of this proposed interpretation letter was still uncertain.
Healthcare Providers Other than Physicians
A third trend has been growth in the size of the workforce of many healthcare professions. Linked to this has been the expansion of the scope of practice for these professions, which has allowed them to provide more healthcare services to patients outside the restrictions of the CHA. The profession of nurse practitioner has been particularly notable. Between 2012 and 2021, the number of nurse practitioners in many provinces doubled, while the growth in the number of nurse practitioners between 2020 and 2021 alone grew by 10.7 percent (CIHI 2021). At the same time, the scope of practice for nurse practitioners has expanded significantly.
When nurse practitioners were introduced in Canada in 1967 to work in the Northwest Territories, they did not have the authority to practice autonomously and were required to work under the supervision of physicians. By the 2000s, the profession had become self-regulating across all Canadian provinces, although the tasks permitted were quite restricted (Alden-Bugden 2019). Influenced by widening scopes of practice in the United States, the profession by 2023 enjoyed a very wide scope of practice, although this varies from province to province (CIHI 2020). These practices include conducting advanced assessment and diagnosis, ordering and interpreting tests, referring to and consulting with other healthcare providers, prescribing drugs (including controlled substances), admitting patients to LTC facilities, performing invasive and non-invasive procedures, and enjoying full hospital privileges. While these scopes of practice are set by the regulatory colleges, they may or may not be recognized by provincial legislation. They may also require training to show proof of competence, or be restricted by employment contracts. At the inception of the CHA, nurse practitioners were a small workforce with very restricted terms of practice. That the number of nurse practitioners has expanded so dramatically, as has their scope of practice, has meant that they often perform a role very similar to general practitioners. The next section discusses the implications that this has for the provision of private healthcare.
Other professions too are experiencing widening scopes of practice and, in some jurisdictions, these expanded services are being insured publicly in order to increase access to publicly insured services within the public sphere. In addition, with improved access to electronic records, non-physician healthcare professionals, equipped with a full knowledge of a patient’s condition and prescription history, are more able to effectively treat patients (Raiche et al. 2020). For example, pharmacists in many provinces are able to renew, adjust, or substitute prescriptions and may, for some conditions, prescribe drugs, order and interpret diagnostic tests, and administer injections (Tannenbaum and Tsuyuki 2013). The treatment of minor conditions (such as urinary tract infections), the renewal of existing prescriptions, and even the new prescribing of drugs (such as contraceptives) by pharmacists has been added as an insured service in many jurisdictions to facilitate access to basic primary healthcare. In British Columbia, for example, pharmacists can now diagnose and issue prescriptions for 21 minor ailments, including acne, allergies, indigestion, shingles, and urinary tract infections. They can also prescribe contraceptives, and can renew prescriptions for those without a family doctor (Joannou 2023). Similarly, paramedics in some regions have an expanded scope of practice, allowing them to carry out minor procedures. In Halifax, paramedics have played a key role since 2009 in the emergency department of the province’s largest hospital, including suturing wounds, sedating patients, and making casts for broken limbs (Pretty 2018).
The key issue here is the positioning of these other healthcare professions with regard to the legislated restrictions on the private sector. An increased number of non-physician healthcare providers, as well as their expanding scopes of practice, is viewed by many jurisdictions as an efficient means of increasing public access to healthcare services in a context where so many Canadians cannot find primary health providers. This was especially pronounced during the COVID-19 pandemic, when provinces issued care directives expanding scopes of practice for many health professions. But these healthcare providers do not always face the same legislated restrictions against working in the private sector that physicians do. As the next section outlines, the combination of more healthcare providers with widening scopes of practice, technical advances in providing off-site and non-face-to-face healthcare, the growing capacity and expertise of private healthcare organizations in Canada utilizing these professions and this technology, and the critical shortage of traditional physician- and hospital-based care, have begun to change the contours of for-profit healthcare services in Canada.
The CHA, Provincial Health Legislation, and the Parameters of Private Healthcare in Canada
The CHA (and its predecessors) was designed to address a much different healthcare landscape than the one we have now. This section examines the disconnect between the empirical realities of healthcare demand and supply, and the legal frameworks that regulate them. The CHA has, to a remarkable degree, incentivized provinces to shape healthcare within their respective jurisdictions in a manner similar enough that we can in fact refer to a Canadian healthcare system. But this federal statute has no direct legal force on provinces; it merely has the status of a voluntary contract stipulating the terms of receiving federal funding. When we talk about “CHA compliance,” we simply mean that provinces meet the expected terms of the “contract” between parties set out in the CHA. The CHA is only legally binding on the federal government, and only legally requires the Minister of Health (as set out in section 20) to impose penalties in cases where provinces permit either user fees or extra-billing (as per sections 18 and 19). Whether Ottawa chooses to penalize provinces for being non-compliant with the CHA beyond user fees and extra-billing remains subject to its discretion and, to date, successive federal governments have been reluctant in going down this path. This is why the discussion of parallel private services that do not involve user fees or extra billing can be so difficult to understand within the context of the CHA.
CHA Compliance and Indirect Coverage
The CHA is comprised of several different elements. First there are the five criteria (sections 8 to 12) that set out the general requirements that provincial health systems must accept to qualify for federal transfer funding (public administration, comprehensiveness, universality, portability, and accessibility). Then there are the conditions stipulating both that provinces must provide relevant information about their respective healthcare systems to the Canada Health Act Division of Health Canada, and that they must recognize federal financial contributions (sections 13A and 13B). The provisions against extra billing (section 18) and user fees (section 19) mandate Ottawa (under section 20) to impose penalties for non-compliance. Finally, there are the various letters of interpretation (the 1985 Epp letter, the 1995 Marleau letter, and the 2018 Petitpas Taylor letter).
Provincial healthcare legislation has evolved to accommodate the requirements set out in the CHA but, as we have seen, it varies across jurisdictions. As Health Canada has steadfastly withheld federal funding in response to reported cases of extra-billing and user fees, provinces over time introduced measures in their respective legislation proscribing these practices. However, what happens when provinces appear to be non-compliant with sections of the CHA other than extra-billing and user fees is perplexing. One issue in many provinces (excluding Ontario) is whether, or the extent to which, they are compliant with section 9 of the CHA (comprehensiveness). This section states that
[i]n order to satisfy the criterion respecting comprehensiveness, the health care insurance plan of a province must insure all insured health services provided by hospitals, medical practitioners or dentists, and where the law of the province so permits, similar or additional services rendered by other health care practitioners [emphasis added].
Legislation in all provinces except Ontario explicitly states that physicians can offer these services privately. If all insured services provided by medical practitioners must be covered publicly, then how is the private provision of publicly listed services in nine provinces compliant with section 9 of the CHA? As described above, Health Canada distinguishes between “non-participating” and “opted-out” physicians (although there is, as noted in Table 2, inconsistency in the application of these categories across jurisdictions). As services provided by non-participating physicians are not considered to be “insured services,” they are not subject to the provisions of the CHA. Services provided by physicians operating by Health Canada’s definition of “opted-out” are insured services (covered by public plans), and patients can seek reimbursement for services provided. Opted-out physicians are required to inform patients before consultation that up-front payment will be required from them, and these physicians are also required to provide receipts of service. Patients then submit these receipts to the public insurer, which will reimburse them up to the set public fee schedule (excepting Manitoba, where claims for services are forwarded to the public insurer by the physicians).
The difficulty is in identifying how the nine provinces define these categories. Not all accord with Health Canada’s understanding of “non-participating” versus “opted-out.” In New Brunswick, for example, a “non-participating” practitioner is defined in the regulations as one practicing outside of the provisions of the provincial act and, as per Health Canada’s definition of “non-participating,” their patients are not entitled to reimbursement. In Newfoundland, in contrast, while non-participating physicians also are considered to practice outside of the provincial act, their patients are entitled to reimbursement from the province. Nova Scotia does not reference the terms “participating” or “opted out” at all, and merely refers to providers choosing to collect fees for insured services other than through the public insurance system. Prince Edward Island does differentiate between “non-participating” and “participating but opted-out” physicians, but patients in both groups can claim reimbursement from the province. In British Columbia, “enrolled” physicians can request direct payment from patients, whom the province will reimburse (so presumably within Health Canada’s definition of “opted-out”), but as no mention is made of non-enrolled physicians, presumably they can also bill patients directly but their patients will not be reimbursed. Quebec makes a distinction between physicians who are “non-participating” and those who have “withdrawn”; patients of the latter are reimbursed, but patients of the former are not. Alberta uses the term “opted-out,” but this seems to align with Health Canada’s definition of “non-participating,” as patients will not be reimbursed fees made to opted-out physicians. All of these distinctions are noted in table form in Table 2.
This definitional confusion is one reason why compliance with the CHA is so difficult to determine, but is generally understood to those administering these plans and the CHA. Newfoundland’s health insurance act explicitly notes that non-participating physicians are outside of the act, but nonetheless stipulates that patients of non-physicians receiving insured services will be publicly remunerated. PEI goes a step further and makes the distinction between non-participating and opted-out physicians, but supports remuneration for both categories. This would seem to be problematic given the definitions provided by Health Canada. Nonetheless, as there are simply no physicians working outside of the public system in either province, there are no actual instances of non-compliance. Interestingly, Health Canada stopped publishing definitions of “non-participating” and “opted-out” in its CHA Reports after 2020. In total, six of the nine provinces permitting the reimbursement of privately provided insured services do not currently have any physicians working outside of the public insurance system. Thus, while the legislation does permit individuals to access publicly insured services privately, in practice this has been quite rare in most provinces. Quebec, with 642 physicians working outside the public insurance system is a notable anomaly (Table 1).
Why have so few physicians taken advantage of the provision allowing them to practice privately, especially when their patients can enjoy reimbursement of any fees for publicly insured services? It is because most jurisdictions permitting this option limit the fees that physicians can use.
They stipulate that any fees charged by physicians billing directly cannot exceed those on the public fee schedule. In this way, physicians have no financial incentive to seek employment outside of the public insurance system (which is why the Cambie plaintiffs challenged provisions within BC’s Medicare Protection Act that restricted billings to the public fee schedule for enrolled and opted-out physicians). PEI does not impose caps on fees, but the population base is so sparse that even higher fees would likely not enable a private practice to be commercially viable. Saskatchewan and Quebec do allow higher fees, but only under certain conditions.
CHA Compliance and Provincial Definitions of Insured Services and Providers
Parallel private care has also increasingly been provided by clinics in a number of provinces where up-front payment can be tendered for publicly insured services that will not be reimbursed by public insurers. How is this practice CHA-compliant? Again, much depends on the definition of “insured services”. If services provided by non-participating physicians are uninsured by definition, then they are CHA compliant. But there is another definitional provision that can turn “insured services” into uninsured ones. For example, some clinics are generally staffed by healthcare providers other than physicians. As noted above, the scopes of practice of other healthcare providers (notably, but not exclusively, nurse practitioners) has meant that private healthcare clinics are increasingly staffed by nurse practitioners (or nurses supervised by nurse practitioners). Scopes of practice for nurse practitioners vary across provinces but they now tend to be quite substantial. This means that nurse practitioners can provide an array of services that closely match that of GPs, while at the same time in some provinces they are not limited by any provincial legislation stipulating that medical practitioners must adhere to the public fee code. This is possible because, while the CHA stipulates that “all insured services” must be covered publicly, some provinces define “insured services” as “services provided by physicians” (Table A2). Some provinces include specific services provided by dental surgeons and optometrists within the rubric of “insured services”; Nova Scotia specifies that dentists and optometrists providing specific insured services are deemed to be physicians “for the purpose of the plan.” Note that the wording in provincial legislation differs significantly: in Newfoundland regulations, only a physician is deemed to be a “practitioner”; Prince Edward Island’s statute stipulates that a “practitioner” only refers to healthcare professionals other than physicians; and Manitoba’s legislation considers both physicians and any other provider of insured services to be “practitioners.”
The strategy of defining insured services as “only services provided by physicians” did not have much impact when the numbers of non-physician healthcare providers were small, with very restricted scopes of practice. As these have both expanded, nurse-practitioner-run clinics are increasing, and they are able to perform similar services to GPs. Unlike GPs, however, they can in some provinces charge as much as they like for these services. Depending on provincial laws, physicians could plausibly partake in this unregulated private healthcare market by hiring nurses and nurse practitioners, and billing privately for these publicly insured service in excess of the public fee schedules. As these physicians would merely be acting in their capacity as entrepreneurs, rather than providing services directly, they would not be in violation of provincial legislation limiting physician fees to the public fee schedule.
As noted above, two broad trends have, in tandem, reduced the effectiveness of provincial measures constraining parallel private care. The first comprises supply-side factors: there is now a growing cadre of healthcare professionals who can provide services often free of the constraints imposed upon physicians. The second factor is demand-side: if people have immediate access to their GPs, without any upfront payment, they will of course have little incentive to seek the services of nurses or nurse practitioners, potentially at a much higher out-of-pocket cost. But if patients cannot access their GP in a timely manner, or if they have no GP at all, then immediate access to a nurse practitioner, even at higher cost, becomes very attractive.
There are some legal hurdles to the provision of private care by non-physicians that, again, generally vary from province to province. While nursing scopes of practice are rather vague and overlap with physicians’ scopes of practice in primary care, the provincial colleges of physicians and surgeons nonetheless serve as the de facto governing bodies and can determine what is or is not allowed when any other health profession’s scope of practice overlaps with theirs (for example, they may stipulate controlled acts that can only be performed by certain kinds of physicians). Another indirect limitation to private nurse- or nurse practitioner-run clinics may be the willingness of commercial insurers to ensure liability for these professions operating at the full extent of their legal scopes of practice.
There is an assumption that section 9 of the CHA requires “all” medically necessary services provided by physicians and hospitals to be publicly insured. Outside of hospitals and physician care, the implication is that services can be provided privately. But, contrary to public understanding, section 9 of the CHA does not stipulate that all services provided by hospitals and physicians must be covered publicly, but rather that all insured services provided by hospitals and medical practitioners must be covered. To the extent that provinces are free to determine what services they choose to insure (set out in the relevant statutes or regulations), they are generally able to remain CHA compliant under section 9 simply by setting out which services are considered insured ones. Interestingly, section 9 of the CHA also specifies that insured services can be provided by other healthcare providers: “where the law of the province so permits, similar or additional services rendered by other healthcare practitioners” must be included. Thus, the CHA does recognize that physicians are not the only healthcare professionals who should be considered as providers of insured services, notwithstanding provincial legislation that defines insured services as “services provided by physicians.”
If greater privatization has been facilitated by increasing numbers of professions with widening scopes of practice who can provide private services that duplicate publicly insured services, then the charge that the CHA is outdated and must be revisited is unsubstantiated. Rather, the ability to constrain or facilitate access to this kind of private healthcare emphatically rests with the provinces. In some provinces, relevant changes can be made at the level of regulations, and so could be executed quite simply through orders-in-council, assuming the political will existed to do so. Saskatchewan has a novel failsafe provision in its Medical Care Insurance Act stipulating that the Governor in Council can limit private access to publicly insured services in any case where it deems that “reasonable access to insured services is jeopardized” because physicians or other persons are providing services privately. The mechanism here is that the publicly insured services provided privately by opted-out physicians are considered by law to be “uninsured services”; but in cases where publicly insured services are “in jeopardy” these “uninsured services” become, via orders-in-council, insured services, and can no longer be provided privately.
To recap, a key trend in the privatization of Canadian healthcare is expanding scopes of practice, and increasing numbers, of non-physician professionals, especially nurse practitioners. This expansion can be salutary in meeting the demands for healthcare within the public sector. But it can, in some jurisdictions, create the opportunity for a parallel system of private healthcare services where access to GPs has become critically limited. Each province has its own basket of regulatory approaches that determine the contours of this private care. Whether private care is expanded or constrained through these regulatory mechanisms will depend on the political priorities of the respective provincial governments.
CHA Compliance Based On Where and How Services are Provided
Another issue influencing parallel private services is the question, not of who provides them, but of where and how. One manifestation of this is the tension between federal and provincial governments over the public insurance of private diagnostic services. When the federal Hospital Services and Diagnostic Services Act was passed in 1957, there was no doubt an expectation that diagnostic services would naturally be provided within hospitals because of the expense and specialized nature of the equipment required. The CHA defines “hospital services” to include “laboratory, radiological and other diagnostic procedures, together with necessary interpretations.” Private free-standing clinics began to emerge when it became apparent that diagnostic tests, including MRI and CT capacity, were a critical aspect of medical practice, and that there was considerable demand for these services not only from hospitals and third-party insurers but also from individual patients. A 2023 CADTH report notes that at least 85 private diagnostic clinics operate in seven provinces: Quebec (with 36 percent of the private clinics), Alberta (21 percent), British Columbia (18 percent), Ontario (16 percent), Saskatchewan (6 percent), New Brunswick (1 percent), and Nova Scotia (1 percent). Almost two-thirds of these clinics (64 percent) operate within a system of chain ownership. They generally specialize in some combination of ultrasound, CT, MTI, SPECT, and PET services. In 2018 less than 10 percent of these services were provided privately, although the planned expansion of private clinics across Canada suggests that this number may be increasing (CADTH 2023).
An important question underlying the federal Diagnostic Services Policy is whether insured hospital services, once they are provided off-site, are no longer insured services. The CHA itself defines “hospital services” as listed services “provided to in-patients or out-patients at a hospital.” In March 2023, federal Minister of Health Jean-Yves Duclos announced “mandatory” deductions totaling over $82 million from provinces considered to have permitted patient charges levied for “medically necessary services that should be accessible to patients at no cost” (Health Canada 2023d). Deductions to provincial health transfers have in the past only been levied in accordance with sections 18 and 19 of the CHA, where Health Canada is mandated to levy fines. Can diagnostics be included under sections 18 and 19? To the extent that diagnostic services are not insured health services when they are not provided in hospitals, they would seem not to fit within this category. However, under the federal Diagnostic Services Policy, in conjunction with the federal Policy on Private Clinics, private clinics delivering “hospital-like” services are considered to be “hospitals” for the purpose of the CHA.
Another complicated area is that of infusion clinics. While private off-site clinics do exist (see Grant 2018), some hospitals will provide on-site infusions of medically necessary pharmaceuticals, using drugs that patients themselves have purchased, despite these drugs being listed in provincial formularies, and despite the use of hospital nursing staff to oversee these procedures. As the CHA states that insured hospital services include “drugs, biologicals and related preparations when administered in the hospital,” this practice would seem to fall under the definition of “user fees.” Yet provinces have the authority to define what constitutes a ”hospital” within their respective jurisdiction. They could arguably determine that particular locations within a hospital structure (e.g., rooms or floors) are not formally part of the “hospital,” and that services provided within them are therefore not insured services under the CHA.
Loopholes also exist based on where services are provided. In Ontario, the stipulation that “insured services” are only those provided within the province of Ontario (unless explicitly authorized otherwise) means that residents are free to travel to provinces with more liberal legislation to seek parallel private services. Grey areas remain regarding the point at which private services provided out of province may require follow-up care in one’s province of residence. As described in the previous section, parallel private services provided virtually by an out-of-province healthcare provider present another challenge to the CHA, both in terms of interpretation (does provincial regulation apply to the province the patient seeking treatment resides in, or the province where the provider is resident?) and in monitoring compliance with provincial legislation and the CHA. Again, the supply/demand dynamics noted with reference to other healthcare providers apply here as well: the private delivery of publicly insured services provided off site, or out of province, becomes commercially viable when the demand cannot be met adequately in the public system. Where contested areas were once functionally unexplored when demand was met in the public sphere, increasingly long wait times will likely compel the expansion of these private services.
Conclusion
The nature and extent of private healthcare provision has always been a subcurrent in discussions of Canadian healthcare. As Flood and Archibald clearly demonstrated in 2001, however, the precise nature of private healthcare depends upon the structure of provincial legislation. In general, provinces with a critical mass of population and wealth had to be more actively restrictive in their policy instruments regarding private healthcare, with smaller provinces able to enjoy a more liberal legal framework safe in the knowledge that low demand would make the opportunity immaterial. While legal frameworks are generally holding firm, the practice and context of healthcare provision have been changing rapidly. Both supply and demand pressures are making private healthcare more available and more attractive to those requiring healthcare.
This Commentary has not discussed the provision of duplicative private health insurance in Canada. The experience of post-Chaoulli Quebec has shown that the demand for duplicative insurance is still limited given the current policy framework (see Quesnel-Vallée et al. 2020). Nonetheless, if private service provision becomes widespread, and the demand remains constant (or increases), provinces that permit private insurance (but have not experienced demand) may well see its tentative development within their jurisdictions, while provinces where duplicative insurance is proscribed may experience greater political pressure to allow it.
Laverdière (2023) has argued that a “plausible interpretation” of the CHA is that “transfer reductions can only occur when the public system in a province or territory does not provide satisfactory access to medically necessary services.” This is not an incorrect observation per se; it merely confuses the legal and political aspects of the CHA. Whether provinces have met the contractual conditions to expect the funds set out by Ottawa is a largely technical matter. The success that Health Canada has had in eliminating extra billing and user fees under sections 18 and 19 is illustrative of the utility of a clear and specific set of requirements that are monitored and enforced (with the added incentive that provinces can recoup any past losses if they make prospective changes). More complicated are the charges that provinces have been non-compliant with the CHA beyond sections 18 and 19. Because provinces have considerable authority in determining key terms like “medically necessary” or “insured services,” it is difficult to make justiciable claims against provinces for non-compliance more broadly. The contest over diagnostic services and virtual care will be an interesting one. But the terms of the dispute are more political than legal. As in the past, the federal government is using the CHA as a political statement to affirm its commitment to public healthcare; as such, the legal outcome of the controversy may be less important than the political battle.
Is the CHA obsolete? The demand that the CHA should be revised, either to prevent or facilitate private healthcare, is misplaced. The instruments determining the extent of private healthcare largely rest, as they always have, with the provinces and the political will of their electorates. In the past, the best barrier to privatization has been an effective and responsive public system. For this reason Ottawa’s role in funding provincial healthcare remains paramount. Provinces have the legislative tools to constrain the growth of private healthcare, if that is their objective. Similarly, provinces have considerable authority to increase the scope of private healthcare, if that is their objective (even within the current parameters of the CHA), by revising provincial legislation or regulation.
Either way, the specific policy direction undertaken would be different for each jurisdiction, as legislation and other barriers to private healthcare (such as market size) vary across provinces. For example, should Ontario wish to expand the private provision of healthcare, it could simply rescind sections 15(a) of the Ontario Health Insurance Act and section 10(3) of the Commitment to the Future of Medicare Act (along with the corresponding regulations). To expand the scope of private healthcare, the nine provinces that already allow physicians to opt out of the public insurance system have a number of mechanisms at their disposal. These include permitting physicians to charge above the current fee schedule where that is now explicitly prohibited, reimbursing patients who use private-sector physicians where they do not already do so, or permitting “dual” or “duplicative” insurance where it is currently prohibited. The greatest effect would be in the wealthier and more populous provinces where a critical mass of individuals who would be willing to pay to access these services would make private healthcare a viable commercial venture. The scope for expanding private healthcare in smaller provinces is more restricted, but still could be facilitated by, for example, allowing physicians to bill above the public fee schedule.
Similarly, provinces can use legislative mechanisms at their disposal to further restrict the expansion of private healthcare by, for example, refusing to reimburse patients who have paid physicians directly for services listed as “insured services” (as some already do). Doing so could also potentially expand private healthcare by increasing the number of non-participating physicians (who are outside the purview of the CHA). However, this could in turn be addressed by restricting the fee schedule of non-participating physicians or, like Saskatchewan, by permitting liberal private care only up to the point that it is deemed to undermine public care. Moreover, simply by changing the definition of “insured services” from “medically required services provided by physicians” to “medically required services provided by physicians and nurse practitioners” (which can in some jurisdictions be done through orders-in-council alone), some provinces could forestall the expansion of private nurse-practitioner-run clinics. Provinces can also control the precise scope and nature of additional private healthcare services by tightly regulating the specific terms under which these services are permitted. Quebec, for example, has for years allowed private health insurance only for specific procedures; Saskatchewan permits private health insurance, but only if offered by non-profit entities. Privatization, in this way, does not necessarily entail a “wild west” of unrestricted commercial ventures. At the same time, provinces that pursue this route will also have to commit considerable resources for monitoring and ensuring compliance (where currently most provinces simply utilize a complaint-driven system).
Canada’s unique federal system means that fears of privatization can also be useful in leveraging more funding from Ottawa. Rather paradoxically, provinces have an incentive not to contain the growth of private healthcare within their borders in order to make the case that more public funding is necessary. At the same time, Ottawa has agency with regard to going beyond the mandated provisions of sections 18 and 19. It could demand provinces cleave to the spirit of the CHA by publicly insuring services regardless of whether they are provided in the way they were when medicare was first conceived. Ultimately, however, governments are responsive to their electorates. The legal intricacies that exist in the nexus of provincial legislation and the CHA will always remain secondary to the wider political opposition to, or support for, private healthcare. To engage in this political debate, however, it is important to understand clearly what private healthcare is and is not, and how it manifests within the legislative landscape of each jurisdiction.
1 Tables appear following the references section at the end of the document.
2 This is similar to the categorization of workers’ compensation in Canada where a highly-regulated, not-for-profit form of health insurance is generally considered to be within the “public” category of health expenditure.
REFERENCES
Alden-Bugden, Donna. 2019. “The Role and Scope of the NP in Canada.” The Nurse Practitioner. 44(9): 8-10.
Angus Reid Institute. 2022. “Access to Health Care: Free, but for All?” September. Available at
https://angusreid.org/canada-health-care-issues/
Besley, Timothy, John Hall, and Ian Preston. 1998. “Private and Public Health Insurance in the UK.” European Economic Review (42): 391-497.
Böhm, Katharina, Achim Schmidt, Ralf Götze, Claudia Landwehr, and Heinz Rothgang. 2013. “Five Types of OECD Healthcare Systems: Empirical Results of a Deductive Classification.” Health Policy, 113(3): 258-269. Available at http://dx.doi.org/10.1016/j.healthpol.2013.09.003
Canadian Agency for Drugs and Technologies (CADTH). 2022. Managed Equipment Services. Available at https://www.cadth.ca/sites/default/files/attachments/2022-09/managed_equipment_services.pdf
______________. 2023. “Privately Operated Medical Imaging Facilities Across Canada.” Canadian Journal of Health Technologies 3(5). Available at https://canjhealthtechnol.ca/index.php/cjht/issue/view/30
Canadian Institute for Health Information (CIHI). 2020. Nurse practitioner scopes of practice vary across Canada's provinces and territories. Available at https://www.cihi.ca/en/nurse-practitioner-scopes-of-practice-vary-across-canadas-provinces-and-territories
______________. 2021. Data tables: Nurse Practitioners. Available at https://www.cihi.ca/en/nurse-practitioners#:~:text=In%202021%2C,the%20NP%20supply%20in%20Canada.
Canadian Medical Association (CMA). 2023. Physician Data Centre. Available at https://www.cma.ca/research-and-policies/physician-data-centre
Day, Brian. 2023. “Private Facilities Will Bring Much Needed Competition to Canadian Health Care.” Globe and Mail, January 20. Available at https://www.theglobeandmail.com/opinion/article-private-facilities-will-bring-much-needed-competition-to-canadian/.
Deber, Raisa. 2003. “Delivering Health Care Services: Public, Not-For-Profit, or Private?” Discussion paper #17 for the Commission on the Future of Health Care in Canada. The Romanow Commission. Available at https://publications.gc.ca/collections/Collection/CP32-79-17-2002E.pdf
DoctorsNS. 2023. 2023 Negotiations Strategy: Member Study – Final Report. Available at https://doctorsns.com/sites/default/files/2023-01/negotiations/negotiations-survey-report2023.pdf
Duckett, Stephen J. 2005. “Private Care and Public Waiting.” Australian Health Review 29(1): 87-93.
Duncan, Pamela, Rachel Hall and Kiran Stacey. 2023. “NHS Chiefs Blame Staff Shortages for Record 7.4m People on Waiting Lists in England.” The Guardian, June 8. Available at https://www.theguardian.com/society/2023/jun/08/nhs-chiefs-blame-staff-shortages-record-74m-people-waiting-lists-england
Fierlbeck, Katherine, and Gregory P. Marchildon. 2023. The Boundaries of Medicare: Public Health Care beyond the Canada Health Act. Montreal and Kingston: McGill-Queen’s University Press.
Flood, Colleen M., and Tom Archibald. 2001. “The Illegality of Private Health Care in Canada.” Canadian Medical Association Journal 164(6): 825-30.
Frangou, Christina. 2023. “How Canada’s Crumbling Health Care System Opened the Door to For-Profit Virtual Care.” Canadian Business, February 15. Available at https://www.canadianbusiness.com/ideas/virtual-clinics-canadas-digital-health-care/
Globerman, Steven. 2020. Understanding Universal Health Care Reform Options: Private Insurance. Fraser Institute. Available at https://www.fraserinstitute.org/sites/default/files/understanding-universal-health-care-reform-options-private-insurance.pdf
Grant, Kelly. 2018. “How a Blockbuster Drug Tells the Story of Why Canada’s Spending on Prescriptions is Sky High.” The Globe and Mail, October 23. Available at https://www.theglobeandmail.com/canada/article-how-a-blockbuster-drug-tells-the-story-of-why-canadas-spending-on/
Ham, Chris. 2007. When Politics and Markets Collide: reforming the English National Health Service. Health Services Management Centre: University of Birmingham. Available at https://www.researchgate.net/publication/237784533_When_Politics_and_Markets_Collide_Reforming_the_English_National_Health_Service
Health Canada. 2023a. Canada Health Act Annual Report, 2012-2022. Available at https://www.canada.ca/content/dam/hc-sc/documents/services/publications/health-system-services/canada-health-act-annual-report-2021-2022/canada-health-act-annual-report-2021-2022-eng.pdf
______________. 2023b. Statement from the Minister of Health on the Canada Health Act. March 10. Available at https://www.canada.ca/en/health-canada/news/2023/02/statement-from-the-minister-of-health-on-the-canada-health-act.html
______________. 2023c. Canada Health Transfer Deductions and Reimbursements – March 2023. Available at https://www.canada.ca/en/health-canada/news/2023/03/canada-health-transfer-deductions-and-reimbursements---march-2023.html
______________. 2023d. “Government of Canada Announces Deductions and Next Steps to Curb Private Health Care Paid Out-of-Pocket.” Available at https://www.canada.ca/en/health-canada/news/2023/03/government-of-canada-announces-deductions-and-next-steps-to-curb-private-health-care-paid-out-of-pocket.html
______________. 2023e. Letter to provinces and territories on the importance of upholding the Canada Health Act. Available at https://www.canada.ca/en/health-canada/services/health-care-system/canada-health-care-system-medicare/canada-health-act/letter-provinces-territories-importance-upholding.html
Hurley, Jeremiah. 2020. ”Borders, Fences, and Crossings: Regulating Parallel Private Finance in Health Care,” in Colleen M. Flood and Bryan Thomas, eds. Is Two-Tier Health Care the Future? Ottawa: University of Ottawa Press, 69-92.
Joannou, Ashley. 2023. “B.C. pharmacists set to treat minor ailments, prescribe contraceptives starting June 1.” Canadian Press. Available at https://www.cbc.ca/news/canada/british-columbia/bc-pharmacists-new-responsibilities-1.6861353
Laverdière, Marco. 2023. “The Canada Health Act Needs To Be Updated.” Policy Options. Available at https://policyoptions.irpp.org/magazines/april-2023/the-canada-health-act-needs-to-be-updated/
Lavergne, Ruth, Sandra Peterson, David Rudoler, David Stock, and Emily Marshall. 2022. “The same, only different: Using physician billing data from four provincial payment systems to describe family physician practice patterns in Canada”. International Journal of Population Data Science, 7(3). doi: 10.23889/ijpds.v7i3.1849.
LeGrand, Julian, Nicholas Mays, and J.A. Mulligan. 1998. Learning from the NHS Internal Market: a review of the evidence. London: King’s Fund.
Lewis, Steven. 2022. “Private Surgeries Will Only Further Fragment Medicare in Canada.” Regina Leader-Post, June 28. Available at https://leaderpost.com/opinion/columnists/lewis-private-surgeries-will-only-further-fragment-medicare-in-canada
Longhurst, Andrew. 2023. Failing to Deliver: The Alberta Surgical Initiative and Declining Surgical Capacity. The Parkland Institute. Available at https://www.parklandinstitute.ca/failing_to_deliver
Marchildon, Gregory. 2020. “Private Finance and Canadian Medicare: Learning from History.” In Collen M. Flood and Bryan Thomas, eds. Is Two-Tier Health Care the Future? Ottawa: University of Ottawa Press.
______________. 2022. “Comparative Healthcare Systems in North America and Europe: Similarities and Differences.” In Katherine Fierlbeck and Joaquín Cayón-de las Cuevas, eds. Health Law and Policy from East to West: Analytical Perspectives and Comparative Case Studies. Pamplona: Thomson Reuters/Editorial Aranzadi S.A.U., 37-54.
McKee, Martin, Nigel Edwards, and Rifat Atun. 2006. “Public-Private Partnerships for Hospitals.” Bulletin of the World Health Organization 84(11): 890-894.
Murphy, Timothy. 2008. “The Case for Public-Private Partnerships in Infrastructure.” Canadian Public Administration 51(1): 99-126.
Naylor, David, Andrew Boozary and Owen Adams. 2020. “Canadian Federal-Provincial/Territorial Funding of Universal Health Care: Fraught History, Uncertain Future.” Canadian Medical Association Journal 192:E1408-12. doi: 10.1503/cmaj.200143
Nova Scotia Health. 2022. Action for Health – Public Reporting. Public Tableau. Available at https://public.tableau.com/app/profile/nova.scotia.health/viz/ActionforHealth-PublicReporting/Overview
Organisation for Economic Co-operation and Development (OECD). 2023. Health at a Glance 20213: OECD Indicators. Paris: OECD Publishing. Available at https://www.oecd-ilibrary.org/sites/7a7afb35-en/1/3/7/5/index.html?itemId=/content/publication/7a7afb35-en&_csp_=6cf33e24b6584414b81774026d82a571&itemIGO=oecd&itemContentType=book#figure-d1e29796-4f0dbe2216
Pretty, David. 2018. “Expanding scope of practice: Paramedics an integral part of QEII’s emergency department.” QEII Times, June 15. Available at https://www.qe2times.ca/expanding-scope-of-practice-232
Quesnel-Valleé, Amelié, Rachel McKay, and Noushon Farmanara. 2020. “Cause or Symptom of Quebec Health System Privatization?” In Colleen M. Flood and Bryan Thomas, eds. Is Two-Tier Health Care the Future? Ottawa: University of Ottawa Press.
Raiche, Taylor et al. 2020. “Community Pharmacists’ Evolving Role in Canadian Primary Health Care: A Vision of Harmonization in a Patchwork System.” Pharmacy Practice 18(4): 2171-2181.
Siemiatycki, Matti. 2015. “Public-Private Partnerships in Canada: Reflections on twenty years of practice.” Canadian Public Administration 38(3): 343-362.
Silver-Greenberg, Jessica, and Katie Thomas. 2022. “They Were Entitled to Free Care. Hospitals Hounded Them to Pay.” New York Times, September 24 (updated 15 December). Available at https://www.nytimes.com/2022/09/24/business/nonprofit-hospitals-poor-patients.html
Tannenbaum, Cara, and Ross Tsuyuki. 2013. “The Expanding Scope for Pharmacists’ Practice: Implications for Physicians.” Canadian Medical Association Journal 185(14): 1228-1231. DOI:10.1503/cmaj.121990
Thomas, Brian. 2020. “Contracting Our Way Around Two-Tier Care? The Use of Physician Contracts to Limit Dual Practice.” In Colleen M. Flood and Bryan Thomas, eds. Is Two-Tier Health Care the Future? Ottawa: University of Ottawa Press.
Vining, Aidan, and Anthony Boardman. 2008. “Public-Private Partnerships in Canada: Theory and Evidence.” Canadian Public Administration 51(1): 9-44.
Wendt, Claus, Lorraine Frisina, and Heinz Rothgang. 2009. “Healthcare System Types: A Conceptual Framework for Comparison.” Social Policy & Administration 43(1): 70-90. DOI: 10.1111/j.1467-9515.2008.00647.x
WHO. 2020. World Health Organization Global Health Expenditure database. Out-of-pocket expenditure (percent of current health expenditure). Available at https://data.worldbank.org/indicator/SH.XPD.OOPC.CH.ZS?locations=CA
Appendix: