Home / Publications / Intelligence Memos / Federal Health Funding: Promises and Performance Gaps
- Intelligence Memos
- |
Federal Health Funding: Promises and Performance Gaps
Summary:
| Citation | Tingting Zhang. 2025. "Federal Health Funding: Promises and Performance Gaps." Intelligence Memos. Toronto: C.D. Howe Institute. |
| Page Title: | Federal Health Funding: Promises and Performance Gaps – C.D. Howe Institute |
| Article Title: | Federal Health Funding: Promises and Performance Gaps |
| URL: | https://cdhowe.org/publication/federal-health-funding-promises-and-performance-gaps/ |
| Published Date: | November 6, 2025 |
| Accessed Date: | November 6, 2025 |
Outline
Outline
Related Topics
Files
From: Tingting Zhang
To: Healthcare observers
Date: November 6, 2025
Re: Federal Health Funding: Promises and Performance Gaps
In Budget 2023, the federal government committed an additional $25 billion over 10 years to fix Canada’s ailing healthcare system, with improved family health services as the first of four shared health priorities.
This investment came with strings attached: Bilateral agreements requiring provinces to set measurable targets, develop detailed action plans, and report progress annually. On paper, it represented a new era of federal accountability for healthcare spending.
Nearly three years later and $7.5 billion disbursed, the results tell a different story.
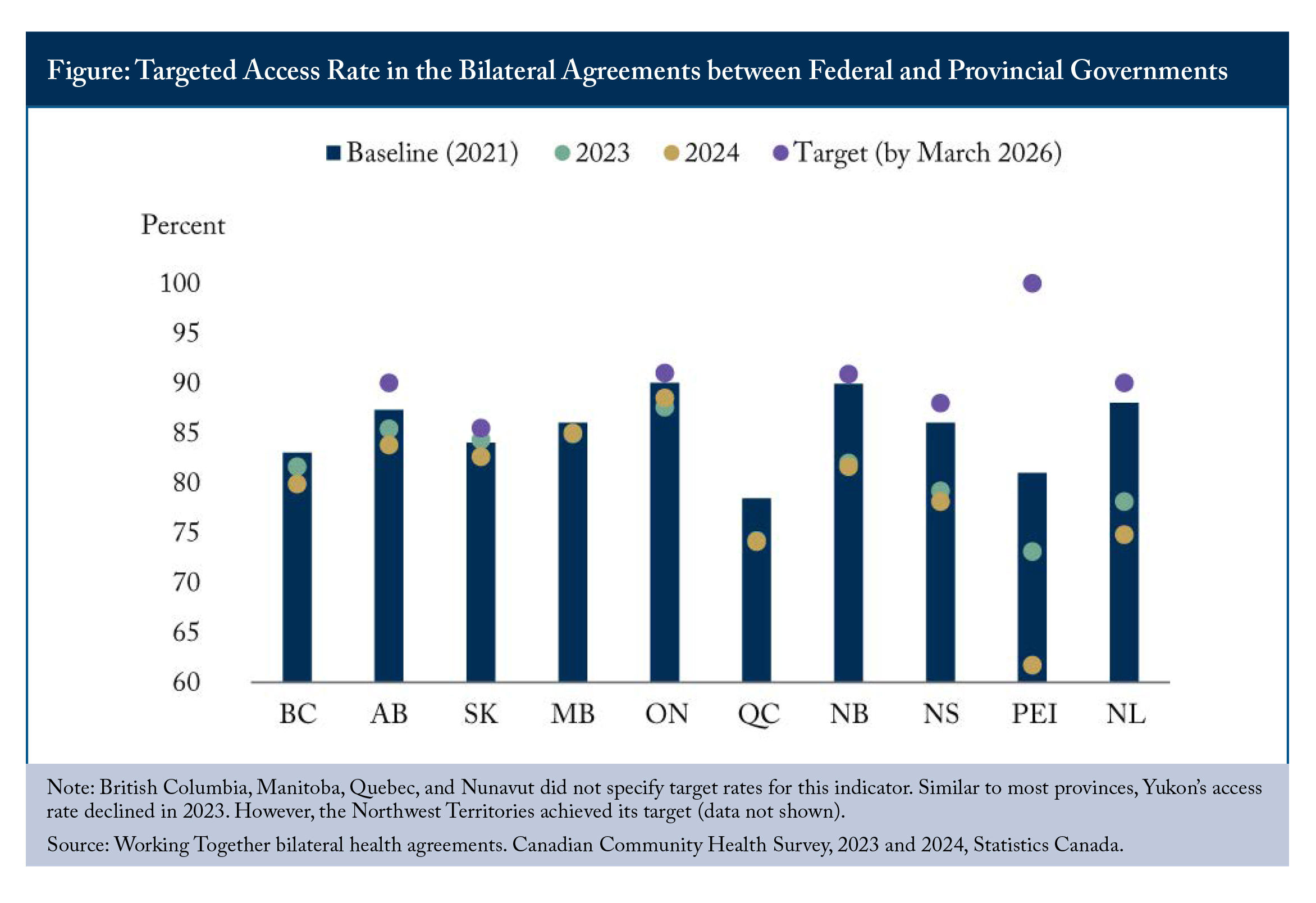
Eight common indicators to track progress were agreed upon, including the percentage of Canadians with access to a regular family doctor, a nurse practitioner, or a family health team. Each province identified baseline rates using 2021 Canadian Community Health Survey data and committed to specific improvement targets by March 2026.
The framework sounds rigorous, but performance keeps deteriorating. Most provinces set modest targets: improving access rates by just one to three percentage points. Yet the 2023 and 2024 Canadian Community Health Survey data reveal that many provinces experienced declining access rates after baselines were established (see Figure). Rather than narrowing the access gap, the distance between current performance and bilateral commitments is widening. This makes the target even more unapproachable.
Ontario, which experienced a 1-percent increase in its access rate between 2023 and 2024, was the only jurisdiction moving in a positive direction. However, its current access rate of 88.5 percent still falls short of its self-imposed target of 91 percent and the 2021 baseline of 90 percent.
Prince Edward Island had the most ambitious commitment to increase primary care access, proposing to raise it from 81 percent to 100 percent by March 2026 – a 19-point jump in three years. While the province has implemented several measures, including building patient medical homes, making better use of pharmacists and streamlined licensing for internationally trained health-care professionals, access continues to decline, with only 61.7 percent of people having a regular primary care provider.
Admittedly, provinces across Canada have been active in improving primary care and addressing family physician shortages. For example, Ontario invested $2.1 billion through its Primary Care Act and supported 130 new and expanded primary care teams. Some municipalities, such as Colwood in British Columbia, hired family physicians as salaried employees to provide primary care for local communities. New Brunswick funded salaries and business costs for interprofessional teams to expand team-based care. Newfoundland and Labrador created publicly funded nurse practitioner positions. Despite extra funding and the rollout of new provincial initiatives, measurable improvements in access have not yet materialized.
A significant evaluation gap also exists. While progress has been reported in some jurisdictions, standardized performance metrics remain inconsistent and apparently uncollected. The Statistics Canada survey was the basis for initial numbers and the provinces generally appear unable or unwilling to release actual numbers.
For example, how many people actually have a primary care provider in each province? How many are on the wait list to be attached to a primary care provider? How many have been connected since new initiatives were introduced? These basic questions remain unanswered except by Statistics Canada’s survey methodology. Without rigorous measurement and transparent reporting, it remains unclear which approaches will prove effective and which initiatives should be scaled up.
A critical challenge has emerged alongside implementation concerns: Shifting federal priorities. The new government has signalled that healthcare may no longer top the policy agenda, while budget pressures threaten sustained funding commitments. To date, $7.5 billion has flowed to provinces and territories under bilateral agreements – but the three-year agreements expire in 2026-27, requiring renewal decisions just as accountability mechanisms face their first real test.
This creates a defining moment for federal accountability: Will Ottawa hold the line or let targets slide?
Federal policymakers face a choice. Despite provincial commitments and significant spending, primary care access remains a significant challenge. Ottawa could pause renewals until provinces demonstrate genuine progress toward intended outcomes, ensuring accountability. However, provinces are unlikely to have the resources to make significant improvements without federal funding, given their own resource constraints. Alternatively, the federal government can continue funding despite missed targets. That would render the accountability framework meaningless, turning it into a failed experiment in conditional funding.
The path forward requires rigorous evaluation of current initiatives and transparent monitoring, not least to let the public see the value of the money being spent on provincial healthcare reforms. Questions such as which initiatives are working, which innovative approaches merit expansion, and where investments should be redirected need to be answered in a timely manner.
Federal funding renewal decisions in 2026-27 must be grounded in an honest assessment of the evidence, even if that means difficult conversations about unmet targets and funding consequences. Conditionality and penalties for non-compliance are hard to enforce. But without such discipline, accountability risks becoming merely performative.
Tingting Zhang is a junior policy analyst at the C.D. Howe Institute.
To send a comment or leave feedback, email us at blog@cdhowe.org.
The views expressed here are those of the author. The C.D. Howe Institute does not take corporate positions on policy matters.
Want more insights like this? Subscribe to our newsletter for the latest research and expert commentary.
Related Publications
- Opinions & Editorials
- Opinions & Editorials

